Decoding PCOS Myths: Separating Fact from Fiction
PCOS is one of the most misunderstood conditions in women’s health. Many people with PCOS are given outdated, ineffective advice—told to just lose weight, go on birth control, or take metformin without any real explanation of what is happening inside their bodies.
I know how frustrating it can be to feel dismissed or misunderstood. When I was first diagnosed, I was given the same advice as everyone else—eat less, exercise more, take these pills. But nothing worked, and no one could explain why. That is what led me to dive into the research, uncover the role of insulin resistance, and develop a science-backed approach that actually works.
Let’s clear up some of the biggest myths about PCOS so you can take control of your health with confidence.
Myth 1: Just Eat Less and Exercise More
For years, I followed the standard advice to cut calories and exercise more, but nothing changed. That is because PCOS is not just a weight problem—it is a metabolic condition driven by insulin resistance.
Most weight loss advice is based on the idea that if you eat fewer calories than you burn, you will lose weight. But if insulin levels are too high, your body is in fat-storage mode, making weight loss nearly impossible.
Fact: PCOS weight loss starts with lowering insulin levels
The key to sustainable weight loss with PCOS is not calorie restriction—it is keeping insulin levels low. Research has shown that lowering insulin helps the body naturally shift into fat-burning mode, making weight loss easier and more sustainable.
This is why a Low Insulin Lifestyle works when other diets fail. Instead of focusing on cutting calories, it focuses on eating foods that support insulin sensitivity:
- Lean proteins like eggs, poultry, and seafood
- Non-starchy vegetables like carrots, tomatoes, and broccoli
- Healthy fats from nuts, seeds, and olive oil
- Whole fruits like apples, pears, and peaches
- Fermented dairy like Greek yogurt and aged cheese instead of milk or whey protein
By keeping insulin low, the body becomes more sensitive to insulin again, breaking the cycle of insulin resistance and making weight loss achievable.
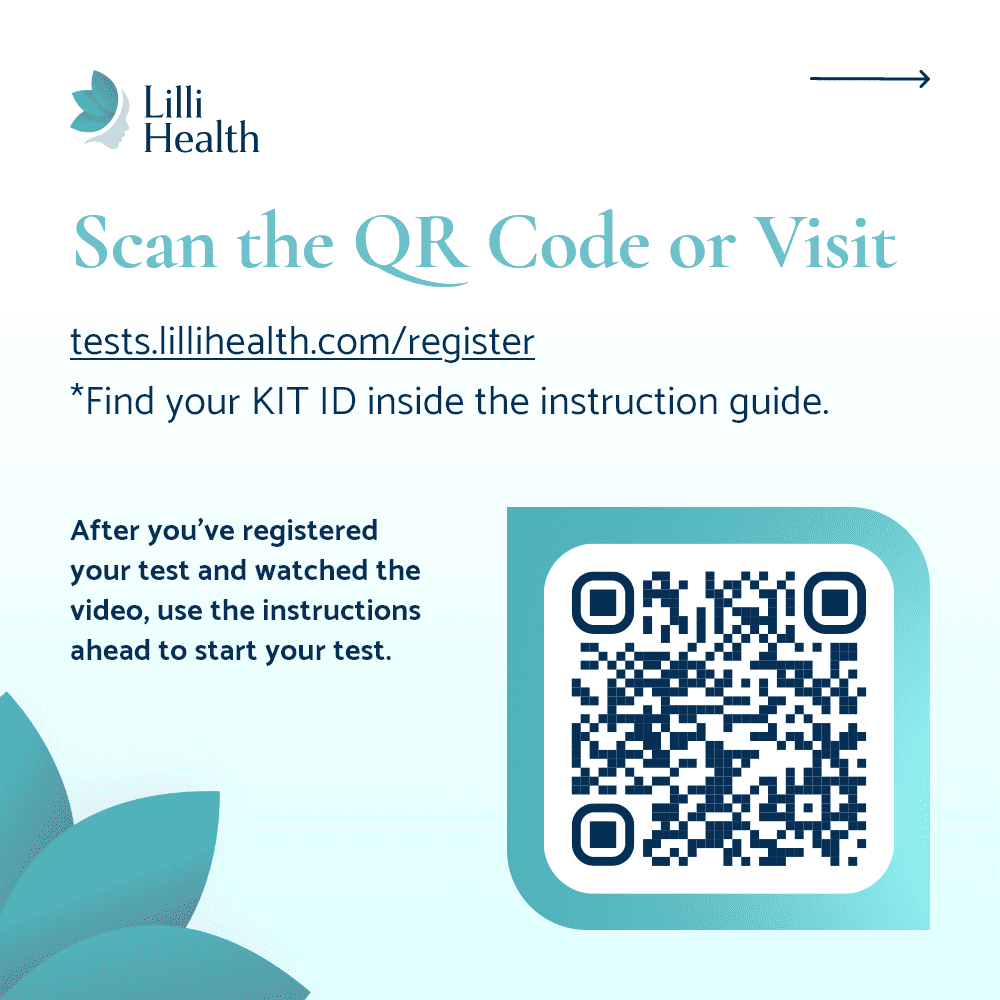
Myth 2: Hemoglobin A1c and Glucose Monitors Test for Insulin
Doctors often use Hemoglobin A1c or Continuous Glucose Monitors (CGMs) to assess metabolic health, but these tests do not measure insulin levels. Many people with PCOS have normal blood sugar but high insulin levels for years before blood sugar is affected.
Fact: Insulin testing is essential for understanding PCOS
Insulin resistance is the root cause of PCOS for most people. When insulin levels are too high, the ovaries produce more androgens, leading to symptoms like acne, hair loss, irregular cycles, and infertility.
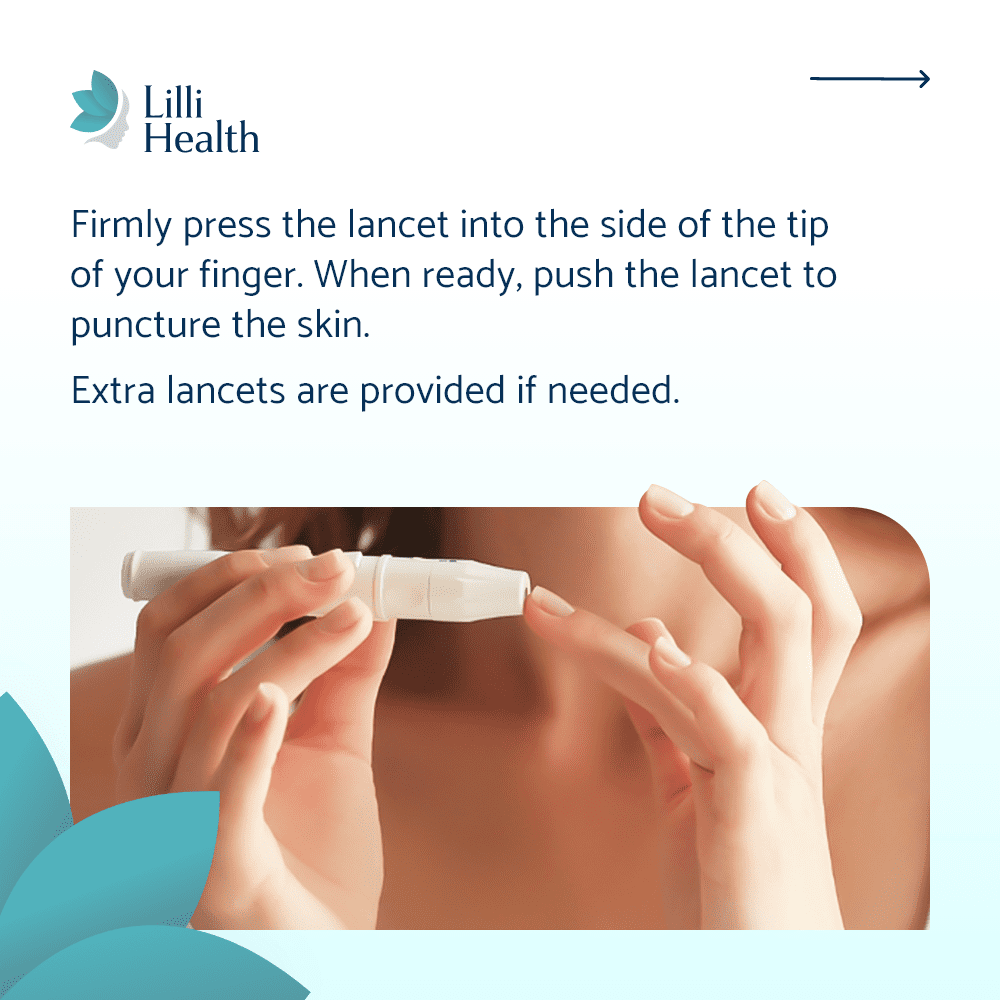
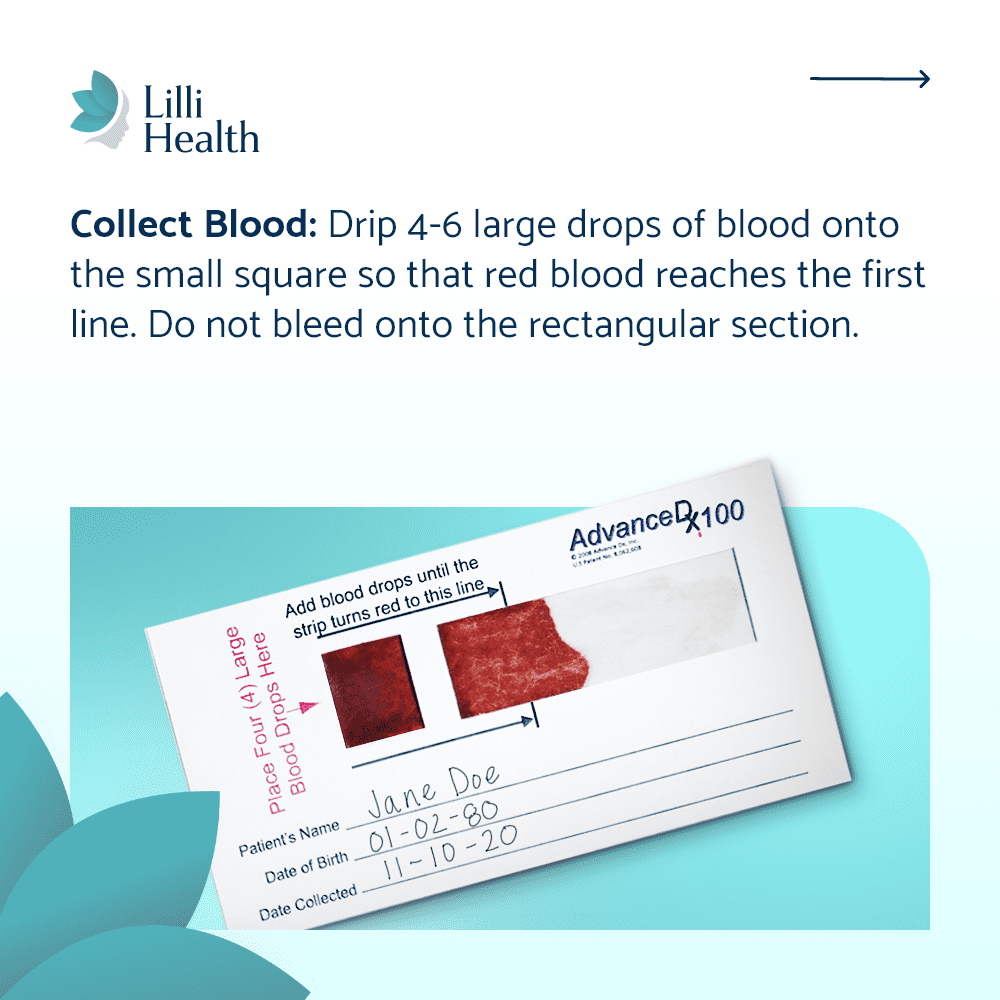
If you want a clear picture of your metabolic health, testing insulin is critical. Since most doctors do not routinely check insulin levels, I created Lilli At-Home Insulin Testing Kits, allowing you to measure fasting and post-meal insulin levels from home.
Myth 3: Birth Control Causes or Cures PCOS
Birth control is one of the most common treatments for PCOS, but it does not cause or cure the condition. While it can help regulate cycles and reduce symptoms like acne and excess hair growth, it does not address the underlying metabolic issues driving PCOS.
Fact: Birth control can help with symptoms but does not treat the root cause
Birth control works by overriding the body’s natural hormonal fluctuations. It can regulate periods, lower androgen levels, and reduce the risk of endometrial cancer in people with irregular cycles.
However, once birth control is stopped, symptoms often return—sometimes worse than before. That is because it does not address insulin resistance, the true driver of hormonal imbalances in PCOS.
For lasting improvements, a Low Insulin Lifestyle can help regulate cycles naturally by lowering insulin and reducing excess androgens.
Myth 4: PCOS Means You Can’t Get Pregnant
Many people with PCOS worry that they will never be able to conceive. While PCOS is the most common cause of ovulatory infertility, it does not mean pregnancy is impossible.
Fact: A Low Insulin Lifestyle can improve fertility
High insulin levels interfere with ovulation, making conception more difficult. By lowering insulin, ovulation can become more regular, improving fertility naturally.
- Studies show that lowering insulin improves egg quality and increases chances of pregnancy
- Many people with PCOS who follow a Low Insulin Lifestyle restore ovulation without fertility treatments
- If medical interventions are needed, reducing insulin resistance first can improve IVF success rates
Fact: Insulin resistance can increase miscarriage risk
Even after conception, high insulin levels can impact implantation and increase miscarriage risk. That is why lowering insulin before pregnancy is so important—it does not just improve fertility, it supports a healthier pregnancy.
Myth 5: PCOS Is Your Fault
One of the most damaging myths is that PCOS is caused by lifestyle choices. Many people with PCOS are made to feel like they did something wrong, but this could not be further from the truth.
Fact: PCOS is caused by genetics and prenatal conditions
Research shows that PCOS develops in the womb. If a fetus is exposed to high insulin or high androgen levels during pregnancy, it can alter gene expression and increase the risk of developing PCOS later in life. This means PCOS can be passed down for at least three generations—meaning your great-grandmother’s metabolic health could be affecting you today.
While you did not cause your PCOS, you do have the power to manage it. By lowering insulin levels, you can break the cycle of insulin resistance, balance hormones, and feel better in your body.
The Bottom Line
The way PCOS has been treated for years is not based on the latest science. The truth is, PCOS is not just a hormone disorder—it is a metabolic condition driven by insulin resistance.
- Weight loss is not just about calories—it is about lowering insulin first
- Blood sugar tests do not show insulin resistance—testing insulin is critical
- Birth control does not treat PCOS—it only manages symptoms
- PCOS does not mean infertility—lowering insulin can improve fertility naturally
- PCOS is not your fault—it starts in the womb, but you can take control of it
If you are ready to stop guessing and start healing, the Lilli App gives you the tools and guidance you need to take control of your PCOS. Inside the app, you will find:
- A research-backed approach to managing PCOS
- Meal plans and recipes designed to keep insulin low
- Tracking tools to monitor insulin, symptoms, and progress
- Education to help you understand what is happening in your body