Hoeger KM, Dokras A, Piltonen T. Update on PCOS: Consequences, Challenges, and Guiding Treatment. J Clin Endocrinol Metab. 2021;106(3):e1071-e1083. doi:10.1210/clinem/dgaa839
Janssen JAMJL. Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int J Mol Sci. 2021;22(15). doi:10.3390/ijms2215779
Macut D, Bjekić-Macut J, Rahelić D, Doknić M. Insulin and the polycystic ovary syndrome. Diabetes Res Clin Pract. 2017;130:163-170. doi:10.1016/J.DIABRES.2017.06.011
Marshall JC, Dunaif A. Should all women with PCOS be treated for insulin resistance? Fertil Steril. 2012;97(1):18-22. doi:10.1016/j.fertnstert.2011.11.036
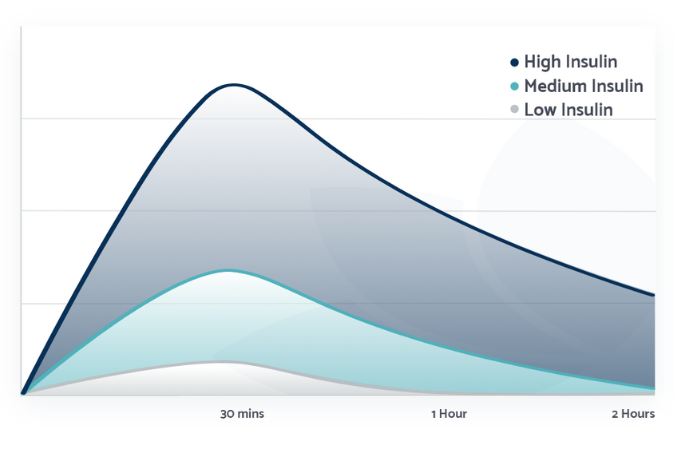
Kravitz E, Dillawn P, Farr MA, Schutt AK. UTILITY OF THE INSULIN CURVE IN ADDITION TO OGTT IN DETECTING HYPERINSULINEMIA IN PATIENTS WITH PCOS. Fertil Steril. 2021;116(3). doi:10.1016/j.fertnstert.2021.07.346
Kravitz E, Dillawn P, Farr MA, Schutt AK. UTILITY OF THE INSULIN CURVE IN ADDITION TO OGTT IN DETECTING HYPERINSULINEMIA IN PATIENTS WITH PCOS. Fertil Steril. 2021;116(3). doi:10.1016/j.fertnstert.2021.07.346
Bell GA, Sundaram R, Mumford SL, et al. Maternal polycystic ovarian syndrome and early offspring development. Human Reproduction. 2018;33(7):1307-1315. doi:10.1093/humrep/dey087
Pohlmeier A. Effect of a Low Insulinemic Diet on Clinical, Biochemical, and Metabolic Outcomes in Women with PCOS. Doctoral Dissertation. Texas Tech University; 2013
Zhang D, Yang X, Li J, Yu J, Wu X. Effect of hyperinsulinaemia and insulin resistance on endocrine, metabolic and fertility outcomes in women with polycystic ovary syndrome undergoing ovulation induction. Clin Endocrinol (Oxf). 2019;91(3). doi:10.1111/cen.14050
Janssen JAMJL. Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int J Mol Sci. 2021;22(15). doi:10.3390/ijms2215779
Macut D, Bjekić-Macut J, Rahelić D, Doknić M. Insulin and the polycystic ovary syndrome. Diabetes Res Clin Pract. 2017;130:163-170. doi:10.1016/J.DIABRES.2017.06.011
Marshall JC, Dunaif A. Should all women with PCOS be treated for insulin resistance? Fertil Steril. 2012;97(1):18-22. doi:10.1016/j.fertnstert.2011.11.036
Kravitz E, Dillawn P, Farr MA, Schutt AK. UTILITY OF THE INSULIN CURVE IN ADDITION TO OGTT IN DETECTING HYPERINSULINEMIA IN PATIENTS WITH PCOS. Fertil Steril. 2021;116(3). doi:10.1016/j.fertnstert.2021.07.346
Jeffery AN, Metcalf BS, Hosking J, Streeter AJ, Voss LD, Wilkin TJ. Age Before Stage: Insulin Resistance Rises Before the Onset of Puberty. Diabetes Care. 2012;35(3):536-541. doi:10.2337/dc11-1281