If you think that worrying about insulin is only relevant to diabetics, think again! Maintaining normal insulin levels is crucial for everyone, regardless of whether they have diabetes or not. It’s not just about preventing insulin resistance; it’s the key to a healthy and fulfilling life, including managing conditions like PCOS.
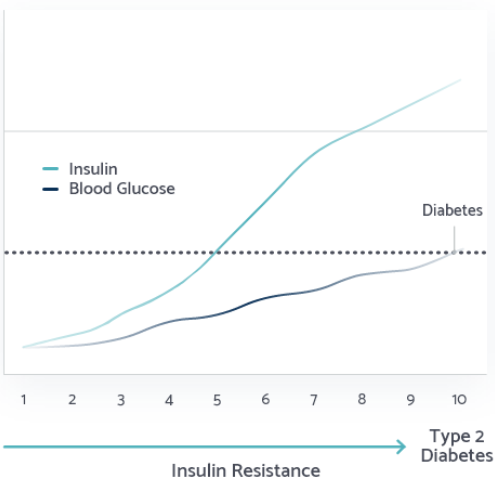
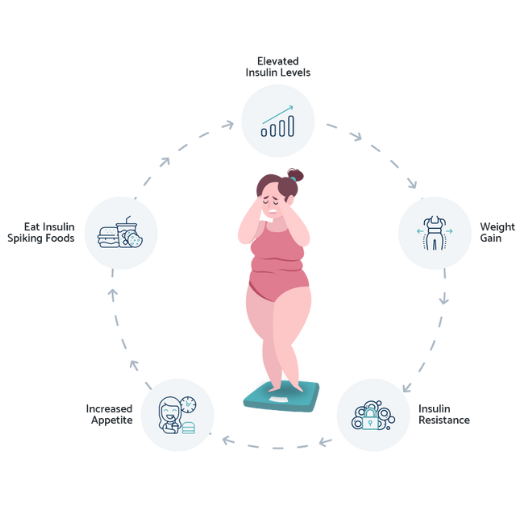
Why is this important? Well, insulin resistance and high insulin levels have been linked to a wide range of health issues, including obesity, type 2 diabetes, heart disease, aging, Alzheimer’s disease, cancer, autism, mood disorders, and infertility. Surprisingly, studies show that 88% of US adults have insulin resistance. What’s even more concerning is that many people may not even realize they are insulin resistant or understand what it means. It’s alarming that insulin resistance, which lies at the core of numerous chronic diseases, isn’t yet a household term.
This is where Lilli Health comes in. Our mission is to educate people about insulin, insulin resistance, and overall health. Lilli, which stands for a low insulin lifestyle, forms the foundation of our company and educational efforts. We strive to inform individuals about the significance of lowering and maintaining normal insulin levels. By doing so, we can reverse insulin resistance, support weight loss, enhance fertility, improve skin complexion, and ultimately lead longer and healthier lives.
At Lilli Health, we believe that understanding insulin and its impact is crucial for everyone, regardless of their health status. Through education and awareness, we hope to empower individuals to make informed choices and embrace a low insulin lifestyle for their overall well-being.