Why Supplements Are Not Always the Answer for PCOS: Addressing the Root Cause with a Low Insulin Lifestyle
For many women with PCOS, managing symptoms often leads to exploring supplements as a solution. It is easy to be drawn in by promises of quick fixes, and common supplements like magnesium and vitamin D are often touted as must-haves. But while supplements can provide short-term relief, they are not always addressing the underlying problem.
In fact, most of the nutrient deficiencies seen in PCOS are actually symptoms of a deeper issue: insulin resistance and chronic inflammation. So before spending money on another bottle of pills, let’s explore why tackling the root cause, rather than just masking the symptoms, is the true way to regain your health.
The Real Reason Behind Nutrient Deficiencies in PCOS: Insulin Resistance
It is no secret that women with PCOS often experience deficiencies in key nutrients like magnesium and vitamin D. What is less commonly known is why these deficiencies occur in the first place.
The answer often lies in insulin resistance, a condition that affects up to 70 percent of women with PCOS. When your body becomes resistant to insulin, your pancreas pumps out more insulin to compensate. This leads to chronically elevated insulin levels, which set off a cascade of problems, including nutrient depletion. Here is how:
- Magnesium Deficiency: High insulin levels cause your kidneys to excrete more magnesium, leading to lower levels in your body. This can worsen insulin resistance and contribute to symptoms like fatigue and muscle cramps.
- Vitamin D Deficiency: In women with PCOS, insulin resistance often leads to weight gain, which causes vitamin D to be stored in fat cells rather than circulating in the blood where it can be used. This further contributes to hormonal imbalances and metabolic dysfunction, worsening the overall effects of PCOS.
The key takeaway? These deficiencies are not isolated problems. They are often symptoms of a deeper metabolic issue: insulin resistance. Addressing insulin resistance is the only way to truly resolve them.
Supplements Are a Band-Aid, Not a Cure
When you take magnesium or vitamin D supplements, you are temporarily boosting your nutrient levels, but you are not fixing the root problem: your insulin resistance. It is like putting a bandage on a wound without addressing what caused the injury in the first place. Sure, you might feel better for a while, but the underlying issues remain unresolved.
This is why supplements often do not deliver the long-term benefits people expect. You are treating the symptom, not the cause, and in many cases, the deficiencies will persist or return.
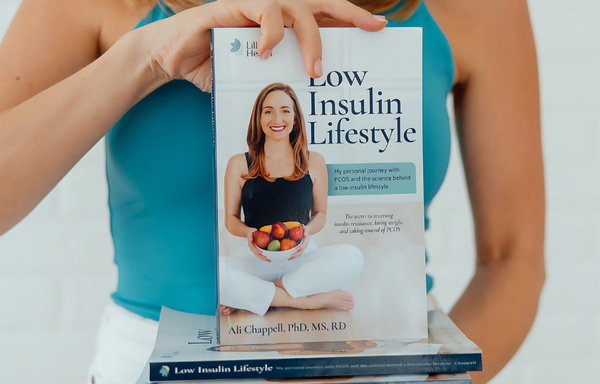
A Low Insulin Lifestyle: The Key to Reversing Nutrient Deficiencies
If supplements are not the long-term answer, what is? The key lies in adopting a Low Insulin Lifestyle, which focuses on lowering insulin levels and reversing insulin resistance through dietary and lifestyle changes.
Here’s why it works:
- Lowers Insulin Levels: By reducing high-starch, high-sugar foods and focusing on nutrient-dense, whole foods, a Low Insulin Lifestyle helps lower insulin levels naturally. This reduces the body’s need to overproduce insulin, addressing the root of the problem.
- Reduces Chronic Inflammation: As insulin levels drop, the inflammation that has been depleting your vitamin D and other nutrients also decreases. This helps your body absorb and utilize nutrients more effectively.
- Prevents Nutrient Depletion: With better insulin sensitivity, your body no longer wastes magnesium and other nutrients through excess excretion, which stabilizes your nutrient levels in the long term.
By addressing insulin resistance at its core, a Low Insulin Lifestyle doesn’t just patch up deficiencies—it helps prevent them from occurring in the first place. This holistic approach leads to sustainable improvements in energy levels, hormonal balance, and overall health, without the need for a long list of supplements.
The Bottom Line
Most vitamin and mineral deficiencies are often the result of insulin resistance and chronic inflammation—issues that supplements cannot fully resolve. To truly tackle PCOS and its associated nutrient deficiencies, focusing on a Low Insulin Lifestyle is key.
By lowering insulin levels and addressing the root causes of your symptoms, you can naturally restore your nutrient balance and improve your overall health—without relying on a handful of pills.
References
- Carrelli A, et al. Vitamin D Storage in Adipose Tissue of Obese and Normal Weight Women. J Bone Miner Res. 2017. Read more
- Barbagallo M, Dominguez LJ. Magnesium and type 2 diabetes. World J Diabetes. 2015. Read more
- Drenthen LCA, et al. Oral magnesium supplementation does not affect insulin sensitivity in people with insulin-treated type 2 diabetes and a low serum magnesium: a randomised controlled trial. Diabetologia. 2024. Read more