Randomized Controlled Trial: Low Insulin Lifestyle vs Standard Advice
For years, women with PCOS have been told to simply eat less and exercise more. They’ve been handed Metformin and told it might help. And when that didn’t work, they were made to feel like they just weren’t trying hard enough. But what if the entire approach was flawed from the start?
That’s exactly what an independent randomized controlled trial (RCT) set out to investigate—comparing the Low Insulin Lifestyle to the conventional advice of calorie restriction, exercise, and Metformin. The results? This lifestyle didn’t just hold its own against standard recommendations—it crushed them.
This wasn’t just any study. It was an independent trial, meaning it wasn’t conducted by us, but by a separate group of researchers. That’s incredibly important because for research to be meaningful, it needs to be replicated by different teams and still show the same results. The fact that an outside group tested this lifestyle and found it to be more effective than conventional advice? That’s huge.
Study Design: A Tough Competitor
This wasn’t a small observational study or a personal success story. This was a randomized controlled trial, the gold standard of research.
Fifty-six women with PCOS were randomly assigned to one of two groups:
-
The Low Insulin Lifestyle Group
- Followed a Low Insulin Lifestyle
- No calorie counting, no portion control, no exercise requirement
- Received either in-person dietary counseling or a web-based education program
-
The Standard PCOS Treatment Group
- Followed conventional medical advice: calorie restriction, increased exercise, and metformin
This was a true head-to-head matchup: a new and unique approach vs. the traditional “eat less, exercise more” plus metformin. Metformin is an incredible medication for lowering insulin, so this was no easy competitor to beat. If our approach even slightly outperformed metformin, that would be groundbreaking.
The Results: A Clear Winner
After just eight weeks, the results showed that the Low Insulin Lifestyle wasn’t just effective—it was more effective than the standard treatment.
-
More Weight Loss Without Calorie Restriction – Women following the Low Insulin Lifestyle lost more weight without having to count calories or restrict portions.
-
Greater Improvement in Blood Sugar and A1c – A1c, a measure of average blood sugar, improved more in the Low Insulin Lifestyle group, showing better long-term glucose control.
-
Better Insulin and Hormonal Balance – Lower fasting insulin and testosterone levels—both major drivers of PCOS symptoms.
- Lower Triglycerides – A Low Insulin Lifestyle significantly reduced triglyceride levels, which shows improved heart health.
-
Web-Based Delivery Worked Just as Well – Women who received the education online saw the same improvements as those who got in-person counseling. This makes the lifestyle accessible and scalable to women everywhere, including through a mobile app.
Why This Matters
This study beat metformin. Let’s pause on that for a second.
Metformin is an amazing drug. Some consider it the fountain of youth. It directly lowers insulin levels, improves insulin sensitivity, and helps regulate blood sugar. It is hands-down one of the best medications that has ever been invented. And yet, a lifestyle approach—eating the right foods without restriction—worked better.
That’s incredible.
And let’s not forget: this lifestyle worked without exercise. Participants in both groups were asked to keep their activity levels the same to ensure diet was the only variable. Despite this, women in the Low Insulin Lifestyle group still lost more weight, improved their metabolic health, and balanced their hormones—all without hitting the gym.
What’s Next?
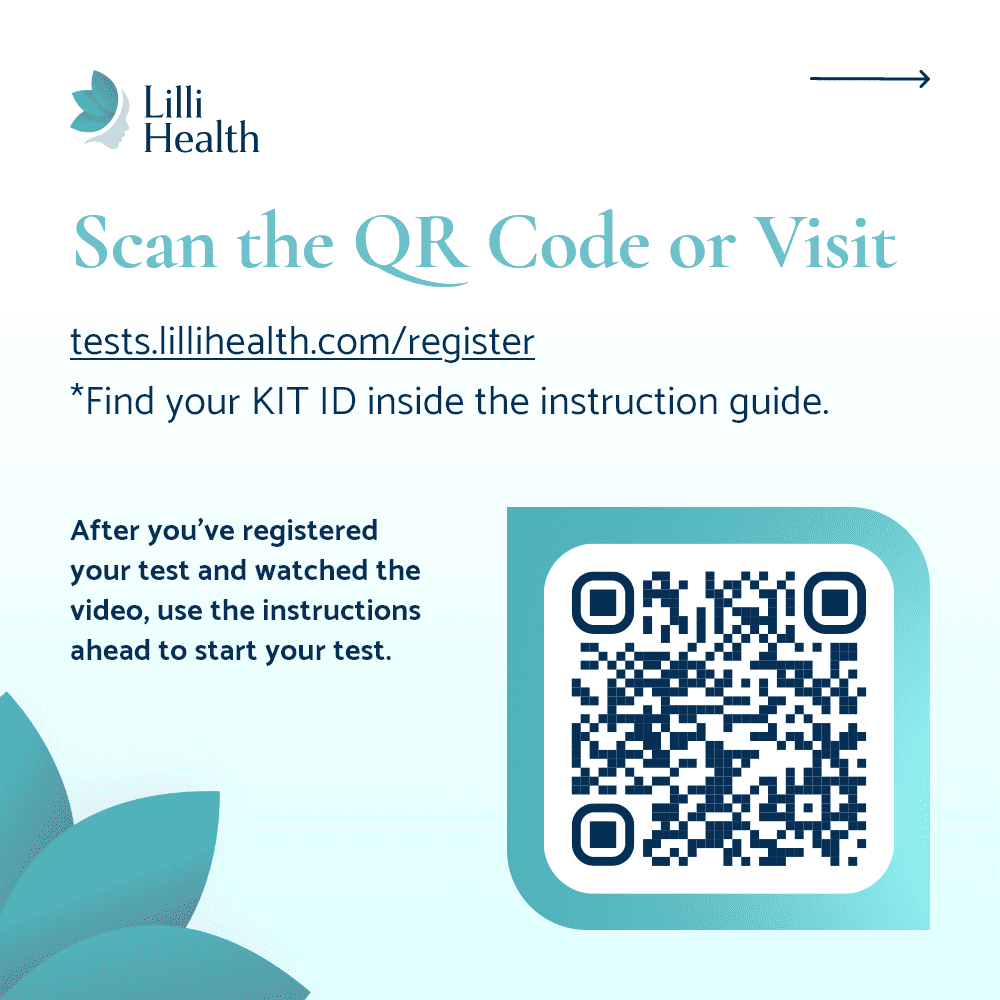
The success of this study laid the foundation for even more research. Next up is the LILACS study, a large-scale randomized controlled trial designed to take everything we’ve learned so far and apply it to a broader population.
LILACS will further validate the impact of the Low Insulin Lifestyle delivered through the Lilli App on insulin resistance, metabolic health, and PCOS symptoms—but on a much larger scale. This study will be a key step toward FDA clearance for the Lilli App, making this approach more widely recognized and accessible.
Each study builds on the last, adding to the growing body of evidence that PCOS is not about eating less and exercising more—it’s about fixing insulin resistance.