Bell GA, Sundaram R, Mumford SL, et al.
Maternal polycystic ovarian syndrome and early offspring development. Human Reproduction. 2018;33(7):1307-1315. doi:10.1093/humrep/dey087
Hoeger KM, Dokras A, Piltonen T.
Update on PCOS: Consequences, Challenges, and Guiding Treatment. J Clin Endocrinol Metab. 2021;106(3):e1071-e1083. doi:10.1210/clinem/dgaa839
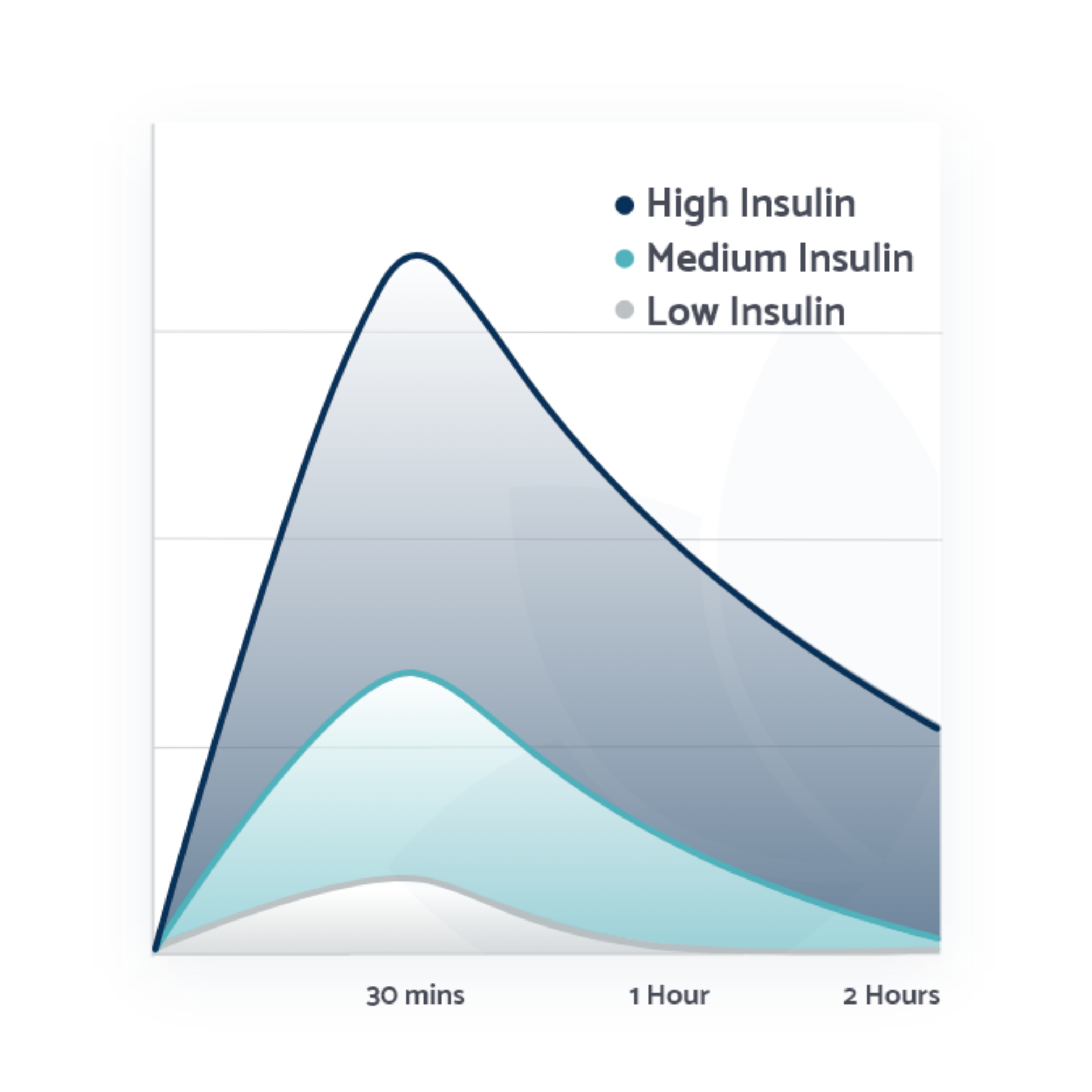
Hopkins D, Chappell A.
Addressing a Key Metabolic Component of PCOS: Insulin. IntechOpen. 2025
Houston EJ, Templeman NM.
Reappraising the relationship between hyperinsulinemia and insulin resistance in PCOS. J Endocrinol. 2025 Mar 12;265(2):e240269. doi:10.1530/JOE-24-0269. PMID: 40013621; PMCID: PMC11906131.
Janssen JAMJL.
Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int J Mol Sci. 2021;22(15). doi:10.3390/ijms2215779
Jeffery AN, Metcalf BS, Hosking J, Streeter AJ, Voss LD, Wilkin TJ.
Age Before Stage: Insulin Resistance Rises Before the Onset of Puberty. Diabetes Care. 2012;35(3):536-541. doi:10.2337/dc11-1281
Kravitz E, Dillawn P, Farr MA, Schutt AK.
UTILITY OF THE INSULIN CURVE IN ADDITION TO OGTT IN DETECTING HYPERINSULINEMIA IN PATIENTS WITH PCOS. Fertil Steril. 2021;116(3). doi:10.1016/j.fertnstert.2021.07.346
Macut D, Bjekić-Macut J, Rahelić D, Doknić M.
Insulin and the polycystic ovary syndrome. Diabetes Res Clin Pract. 2017;130:163-170. doi:10.1016/J.DIABRES.2017.06.011
Marshall JC, Dunaif A.
Should all women with PCOS be treated for insulin resistance? Fertil Steril. 2012;97(1):18-22. doi:10.1016/j.fertnstert.2011.11.036
Melnik BC.
Milk–A Nutrient System of Mammalian Evolution Promoting mTORC1-Dependent Translation. Int J Mol Sci. 2015 Jul 27;16(8):17048-87. doi:10.3390/ijms160817048. PMID: 26225961; PMCID: PMC4581184.
Melnik BC.
Milk consumption: aggravating factor of acne and promoter of chronic diseases of Western societies. J Dtsch Dermatol Ges. 2009 Apr;7(4):364-70. English, German. doi:10.1111/j.1610-0387.2009.07019.x. Epub 2008 Feb 20. PMID: 19243483.
Melnik BC, Schmitz G.
Role of insulin, insulin-like growth factor-1, hyperglycaemic food and milk consumption in the pathogenesis of acne vulgaris. Exp Dermatol. 2009 Oct;18(10):833-41. doi:10.1111/j.1600-0625.2009.00924.x. Epub 2009 Aug 25. PMID: 19709092.
Nilsson M, Stenberg M, Frid AH, Holst JJ, Björck IM.
Glycemia and insulinemia in healthy subjects after lactose-equivalent meals of milk and other food proteins: the role of plasma amino acids and incretins. Am J Clin Nutr. 2004 Nov;80(5):1246-53. doi:10.1093/ajcn/80.5.1246. PMID: 15531672.
Pohlmeier A.
Effect of a Low Insulinemic Diet on Clinical, Biochemical, and Metabolic Outcomes in Women with PCOS. Doctoral Dissertation. Texas Tech University; 2013.
Rogers I, Emmett P, Gunnell D, Dunger D, Holly J.
Milk as a food for growth? The insulin-like growth factors link. Public Health Nutrition. 2006;9(3):359-368. doi:10.1079/PHN2006853
Zhang D, Yang X, Li J, Yu J, Wu X.
Effect of hyperinsulinaemia and insulin resistance on endocrine, metabolic and fertility outcomes in women with polycystic ovary syndrome undergoing ovulation induction. Clin Endocrinol (Oxf). 2019;91(3). doi:10.1111/cen.14050