The Final Stretch: Managing PCOS in the Third Trimester
The third trimester of pregnancy is a time of eager anticipation as you prepare to welcome your baby into the world. If you have PCOS, this final stretch of pregnancy comes with additional considerations, especially when it comes to insulin resistance. Since insulin resistance naturally increases in the third trimester, it is important to manage insulin levels to support both your health and your baby’s development.
How Insulin Resistance Changes in the Third Trimester
Throughout pregnancy, insulin levels naturally rise to help the body store fat for energy. This process ensures that mothers have enough energy reserves to support breastfeeding after delivery. In the third trimester, insulin resistance peaks due to hormonal changes. After birth, insulin levels should drop so the body can begin using stored fat for energy.
However, if insulin levels remain elevated after delivery, it becomes difficult to burn fat for energy, and the brain responds by increasing hunger to compensate for the energy demands of making milk. This is why some women struggle to lose weight postpartum and may even gain weight while breastfeeding. The key to avoiding this is to support insulin sensitivity during the third trimester so that the body can efficiently shift into fat-burning mode after delivery.
Potential Risks of High Insulin Levels in the Third Trimester
- Fetal overexposure to insulin and testosterone. Babies exposed to high levels of insulin and testosterone from mothers with PCOS may experience genetic changes that cause them to overproduce insulin in their own bodies. This can lead to macrosomia, or excessive fetal growth, increasing the risk of complications during delivery.
- Increased risk of macrosomia. When babies grow too large too quickly, they are more likely to experience complications during labor, increasing the chances of needing a cesarean section.
- Higher likelihood of gestational diabetes. Since insulin resistance peaks in the third trimester, many women with PCOS are at an increased risk of developing gestational diabetes. This can lead to high blood sugar levels, preterm birth, and other complications for both mother and baby.
- Elevated risk of preeclampsia. Insulin resistance has been linked to a higher risk of preeclampsia, a condition that causes high blood pressure and organ stress.
Managing PCOS in the Third Trimester
There are several ways to help support insulin sensitivity in the final months of pregnancy to reduce these risks.
- Follow a Low Insulin Lifestyle. Keeping insulin levels in a healthy range throughout pregnancy is critical for preventing complications. This means focusing on nutrient-dense foods that do not spike insulin, such as non-starchy vegetables, lean proteins, fatty fish, eggs, nuts, seeds, and healthy fats. Avoiding starches, added sugars, non-fermented dairy, and whey-based products can help keep insulin levels from rising too high.
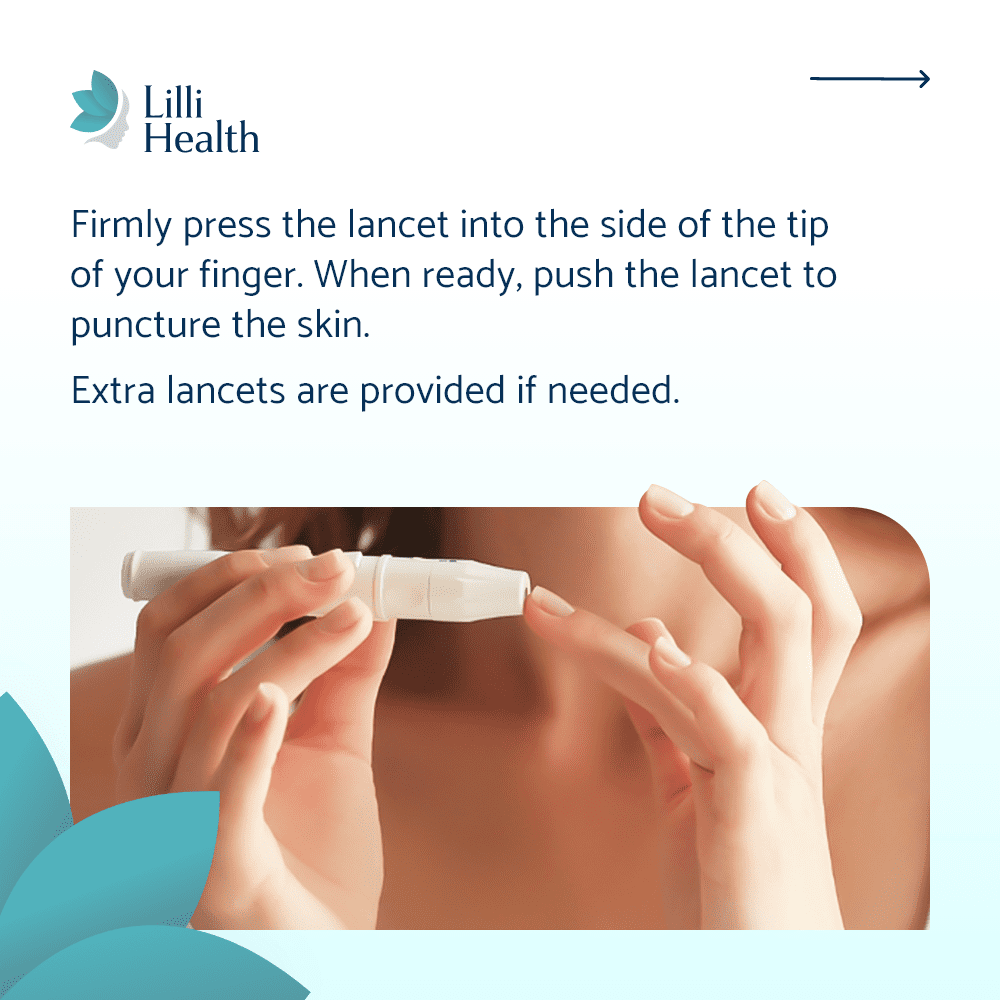
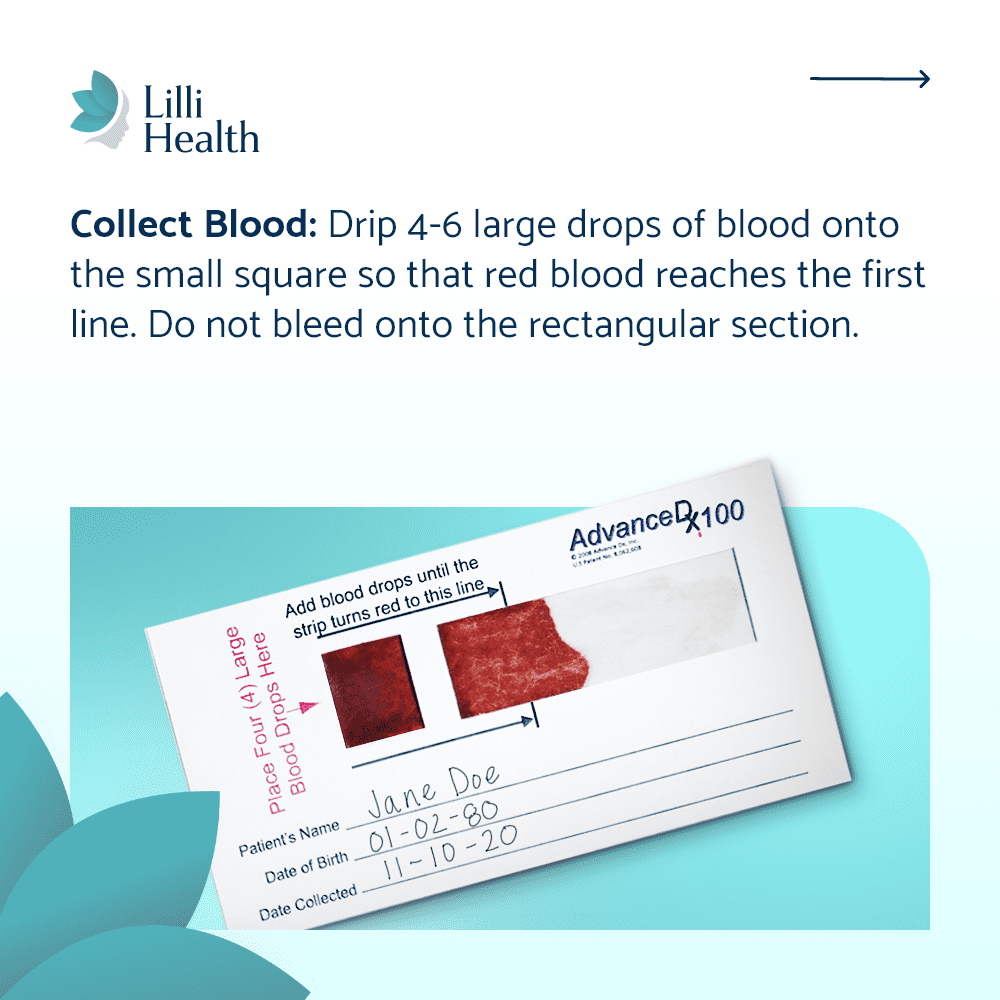
- Monitor insulin sensitivity and blood sugar levels. Regular monitoring allows for early detection of gestational diabetes and helps guide nutrition choices to maintain stable blood sugar. Ask your doctor to order insulin along with glucose during your gestational diabetes screen.
- Incorporate safe movement. Exercise plays an important role in insulin regulation, even in the final trimester. Walking, stretching, and prenatal yoga can help keep insulin levels stable and support better metabolic health leading up to delivery.
- Manage stress. Chronic stress increases cortisol, which can raise blood sugar and insulin levels. Relaxation techniques like mindfulness, deep breathing, or simply taking time to rest can help keep stress in check.
The Final Weeks Before Birth
The third trimester is an exciting time, but it can also feel overwhelming as you prepare for delivery. Taking small, intentional steps to manage insulin levels can make a big difference in how you feel now and in your postpartum recovery.
- Maintaining insulin sensitivity will help your body naturally shift into fat-burning mode after birth, reducing excessive hunger and supporting a healthy postpartum metabolism.
- Managing insulin levels now can improve milk production and help lower the risk of metabolic issues for your baby later in life.
- Staying active and eating in a way that supports balanced insulin levels will help prepare your body for a smoother labor and recovery.
References
Ussar S. Linking maternal obesity to early insulin resistance. Mol Metab. 2014. Read more
Nommsen-Rivers LA. Does Insulin Explain the Relation between Maternal Obesity and Poor Lactation Outcomes? An Overview of the Literature. Adv Nutr. 2016. Read more