Understanding Diabetes: It’s More Than Just High Blood Sugar
When most people hear the word “diabetes,” they think of glucose. But here’s the truth: diabetes isn’t a glucose problem—it’s an insulin problem.
Glucose is just the symptom. Insulin is the driver. Your blood sugar rises because insulin isn’t working properly—or there simply isn’t enough of it. If we want to understand, prevent, or reverse diabetes, we have to stop focusing only on blood sugar and start looking at insulin.
The Different Types of Diabetes
Type 1 Diabetes
This is an autoimmune condition where the body attacks and destroys the insulin-producing cells in the pancreas. People with Type 1 diabetes make little to no insulin and must take insulin injections to survive. It usually starts in childhood but can occur at any age.
Type 2 Diabetes
This is the most common form of diabetes. It happens when the body becomes resistant to insulin or the pancreas can’t keep up with insulin production (or both). Unlike Type 1, it’s often caused by lifestyle factors like diet, weight, and physical activity—but it’s also driven by genetics and other hormonal imbalances like PCOS.
Gestational Diabetes
This type of diabetes develops during pregnancy. Hormonal changes can make cells more insulin resistant, and if the pancreas can’t make enough insulin (or makes too much insulin that doesn’t work) to keep blood sugar in range, gestational diabetes occurs. It usually resolves after pregnancy but increases the risk for Type 2 diabetes later on.
The Many Faces of Type 2 Diabetes
Not all cases of type 2 diabetes look the same. This is important because how your body is handling insulin can guide how to treat it. Here are the three common types I often explain to patients:
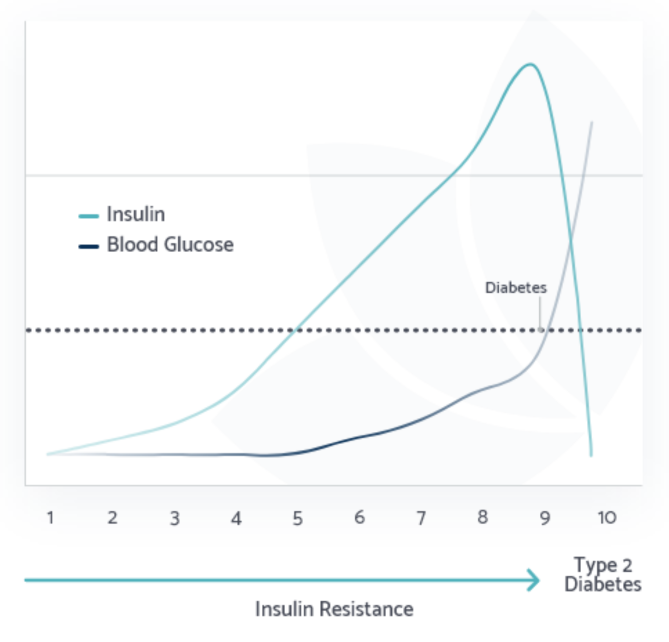
The Workaholic Pancreas
This pancreas is overachieving. It pumps out tons of insulin just to keep blood sugar levels in the “normal” range. This can go on for years before blood sugar starts to rise—so you look “fine” on paper, even though your body is struggling behind the scenes.
What’s really happening?
Your body is becoming more insulin resistant, so the pancreas keeps pumping out more and more insulin to compensate. And insulin is a fat-storage hormone. The more insulin you make, the more likely you are to gain weight.
Key Traits:
- Very high insulin, normal glucose (early stages)
- Often overweight or struggling to lose weight
- Can go undiagnosed for years until the pancreas can’t keep up
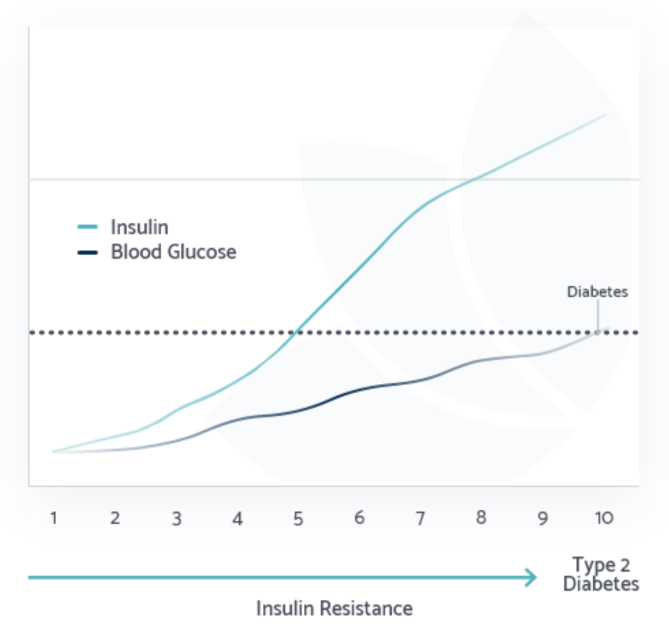
The Retired Pancreas
This pancreas used to be a workaholic—but after years of overproduction, it’s tired. It’s no longer making enough insulin to keep glucose in check. Blood sugar starts to rise. Interestingly, some people in this stage may begin to lose weight—but it’s not a healthy weight loss. It’s a result of insulin deficiency.
What’s really happening?
Your body may have been overweight for decades due to chronically high insulin. But as the pancreas loses function, insulin levels drop, and your body starts to break down muscle and fat—not because it’s healthy, but because it can’t process nutrients properly anymore.
Key Traits:
-
- Long-standing insulin resistance
- Declining insulin production
- May begin to lose weight despite eating normally
- Often signals late-stage Type 2 diabetes
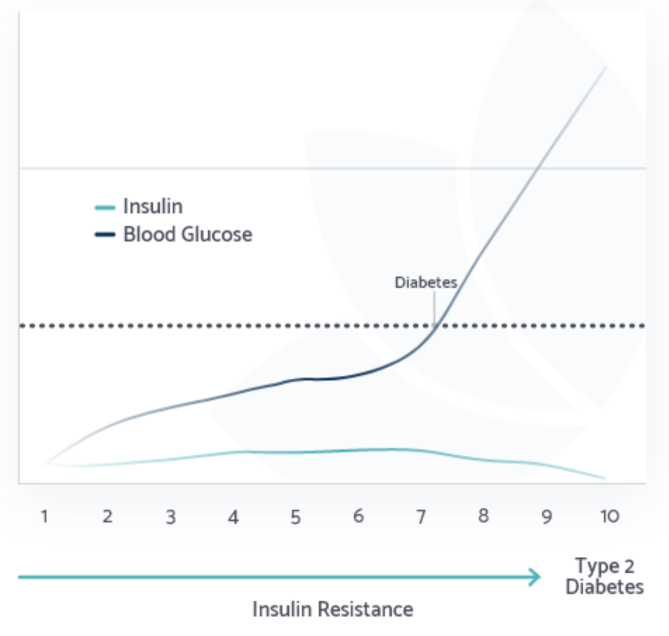
The Lazy Pancreas
This pancreas just doesn’t produce much insulin to begin with. These individuals tend to be naturally lean and may have trouble gaining weight. Their glucose can still rise because there’s not enough insulin to manage even a normal amount of carbs. Eastern Asian populations tend to struggle with a “Lazy Pancreas” because their pancreas can’t keep up with all the starch they eat. It’s also why they tend to be lean yet still have very high rates of type 2 diabetes.
What’s really happening?
These people are often misdiagnosed as having Type 1 diabetes or may be told they’re “the healthy type” because they’re thin. But their inability to make enough insulin creates its own problems, especially with blood sugar control.
Key Traits:
- Naturally lean or underweight
- Low insulin production
- Often misdiagnosed or overlooked
- Sometimes called LADA (Latent Autoimmune Diabetes in Adults)
What We’re Missing in Routine Testing
Here’s one of the biggest problems: all we do in standard medical care is test glucose and A1c. If those are normal, you’re sent on your way with a pat on the back and a “keep doing what you’re doing.”
But this is a false sense of security.
Very few doctors test fasting insulin. And even fewer know how to interpret it. So we wait until glucose is high to act—by then, insulin resistance has been raging silently for years, even decades.
By the time your blood sugar is elevated enough to be flagged as a problem, your pancreas has already been struggling to keep up for a long time. Silently damaging your organs, skin, and tissues.
We’re not testing early enough. And we’re not asking the right questions.
The Problem with How We’ve Been Treating Diabetes
For decades, the medical approach to Type 2 diabetes has been centered around one thing: getting glucose down. But how do most medications do this? By increasing insulin levels—either by making your pancreas release more insulin or by injecting insulin directly.
Here’s the problem: you don’t fix insulin resistance by making more insulin.
You fix it by needing less insulin.
Raising insulin levels may get glucose numbers into the “normal” range, but it worsens the root problem: insulin resistance. It leads to more weight gain, greater dependence on insulin or medications, and, over time, worsened metabolic health—even if your A1c looks better.
The only class of medication that actually works with your body to reduce insulin levels is metformin. But even that can’t do the heavy lifting alone. What you eat every day matters far more.
The Solution: Lower the Need for Insulin
Instead of trying to force your body to make more insulin, the smarter approach is to reduce the need for insulin in the first place.
This means:
- Eating foods that don’t spike insulin
- Giving your pancreas a break from constant insulin stimulation
- Helping your cells become more insulin sensitive
And that’s exactly what A Low Insulin Lifestyle does.
The Bottom Line
Diabetes is an insulin problem with a glucose symptom.
If we keep treating the symptom and ignoring the root cause, we’ll never see real healing.
When we start focusing on insulin—understanding how much is needed, how resistant the body is, and what’s driving the demand—we finally take a step in the right direction. The good news? You can do something about it. And it starts with shifting the way we think. Don’t wait for your A1c to get too high. Ask for your insulin to be tested. Understand what stage you’re in. And take the steps now to change your path forward.
References
Yazbeck AS, et al. How Health Systems World-wide Fail Type 2 Diabetics. Health Syst Reform. 2025. Read more