Want to Improve IVF Success? Start with a Low Insulin Lifestyle
If you’ve been trying to conceive, you’ve probably heard all about egg quality, lining thickness, hormone levels, embryo grading, and transfer timing.
What you probably haven’t heard about? Insulin.
Which is kind of wild, considering it plays a role in every single step of the fertility process—from ovulation to implantation to placental development. Yet almost no one is testing it.
Let’s fix that.
Insulin and Your Fertility: The Missing Link
Insulin is your fat storage hormone, but it’s also a master hormone that influences everything else—including your reproductive system.
If insulin is high (which is shockingly common and often goes undiagnosed), it can interfere with:
- Egg development and quality
- Ovulation timing
- Endometrial receptivity
- Implantation
- Placental formation
- Miscarriage risk
This applies whether you’re trying naturally, using ovulation meds, or doing full IVF.
But Your Doctor Is Probably Not Testing for It
Most fertility clinics check AMH, FSH, estrogen, LH, thyroid, prolactin—all important, but none of those tests tell you what insulin is doing behind the scenes.
A normal A1c or glucose test doesn’t rule out insulin resistance. You could have normal blood sugar and still be:
- Making too much insulin (which affects ovulation and egg quality), or
- Not making enough to keep up with rising hormone demands (which affects implantation and early placental development)
So if you’ve been told “everything looks fine,” but you’re still not getting pregnant—or not staying pregnant—this might be why.
Why PCOS Isn’t Always a Great Candidate for IVF
Here’s something that rarely gets said out loud: people with PCOS are often pushed toward IVF way too soon.
But PCOS isn’t an “infertility problem”—it’s a metabolic problem. And if insulin resistance is at the root (which it is, in the vast majority of cases), then IVF may not work as well as you’d hope.
In fact, research shows that elevated insulin levels are associated with IVF failure, even when everything else looks good. Insulin affects egg quality, hormone balance, endometrial receptivity, and normal placenta development. So if insulin is still high, even the best embryos may not implant.
A group of researchers at Columbia University found that high insulin levels in early pregnancy were as damaging to placental development as chemotherapy drugs. Let that sink in. And yet… measuring insulin isn’t even part of standard fertility care? What. Is. Happening.
The truth is, many women with PCOS can ovulate on their own—without fertility drugs—once their insulin levels come down. Whether that’s through a Low Insulin Lifestyle, metformin, or both, the body often starts doing what it was designed to do.
So if you’ve been told your only option is IVF… pause. Address insulin first. You might not even need it.
Fertility Drugs and Insulin Resistance
Here’s what most people don’t realize: many fertility medications (Clomid, letrozole, injectable gonadotropins) can make insulin resistance worse—especially if it was already there to begin with.
Why? Because these drugs rev up the ovaries and push your body to do more, hormonally speaking. But if insulin is already elevated, or your body is already inflamed, it can make ovulation less predictable, implantation less successful, and the whole process more difficult and expensive than it has to be.
This is exactly why people say things like “I did 3 rounds of IVF and nothing stuck.” It’s not always about the embryos. Sometimes it’s about the hormonal environment they’re being placed into.
What About Rapamycin and Ovarian Aging?
There’s been a lot of buzz lately about rapamycin and its ability to prolong ovarian function and potentially delay menopause. And the research is genuinely exciting—especially if you’re in your 30s or 40s and trying to preserve fertility or improve IVF outcomes.
But here’s what’s important to understand: Rapamycin works by fixing the very problem that insulin resistance causes.
Rapamycin acts on a cellular growth pathway called mTOR—the same pathway that becomes chronically overactivated in people with high insulin levels. When mTOR is always “on,” the body stays in constant growth and stress mode, which can accelerate ovarian aging, egg depletion, and inflammation.
Rapamycin essentially slows that process down by dialing back mTOR and restoring metabolic balance.
But here’s the kicker: You don’t need a prescription drug to start fixing this today. A Low Insulin Lifestyle naturally downregulates mTOR by lowering insulin at the source. You’re supporting the same pathway—without side effects, and with benefits that reach far beyond your ovaries.
So yes, rapamycin is promising. But it’s also a band-aid for a deeper issue: metabolic overload.
Fix the root (insulin), and the system can start to repair itself—no prescription required.
A Low Insulin Lifestyle = Better Odds
Our case series shows this clearly: Patients following a Low Insulin Lifestyle got pregnant in an average of 86 days—with no fertility treatments. These were women with irregular cycles, PCOS, multiple failed attempts, or “unexplained infertility.” And yet, their bodies responded once insulin was under control.
Why? Because this lifestyle lowers insulin levels—by over 50% in just 8 weeks. And when insulin drops, here’s what happens next:
- Supports hormonal balance
- Improves egg quality
- Encourages regular ovulation
- Reduces inflammation
- Creates a more receptive uterine lining
- Promotes healthy placental development
It doesn’t replace medical care—but it makes everything else work better.
If You Have to Do IVF…
Sometimes IVF is necessary, and we’re lucky to have it.
But if you want the best shot at it working the first time, a Low Insulin Lifestyle is your secret weapon.
Because implantation isn’t just about timing—it’s about the metabolic environment.
Egg quality isn’t just about age—it’s about oxidative stress and insulin levels.
Successful pregnancy isn’t just about a positive test—it’s about placental development and staying pregnant.
What You Can (Both) Do Today
If you’re preparing for IVF (or just trying to conceive), start here:
- Reduce starches, sugars, whey protein, and milk (major insulin-spikers)
- Prioritize protein, healthy fats, non-starchy veggies, and whole fruits
- Take a short (or long) walk after meals
- Stop grazing all day—it keeps insulin elevated
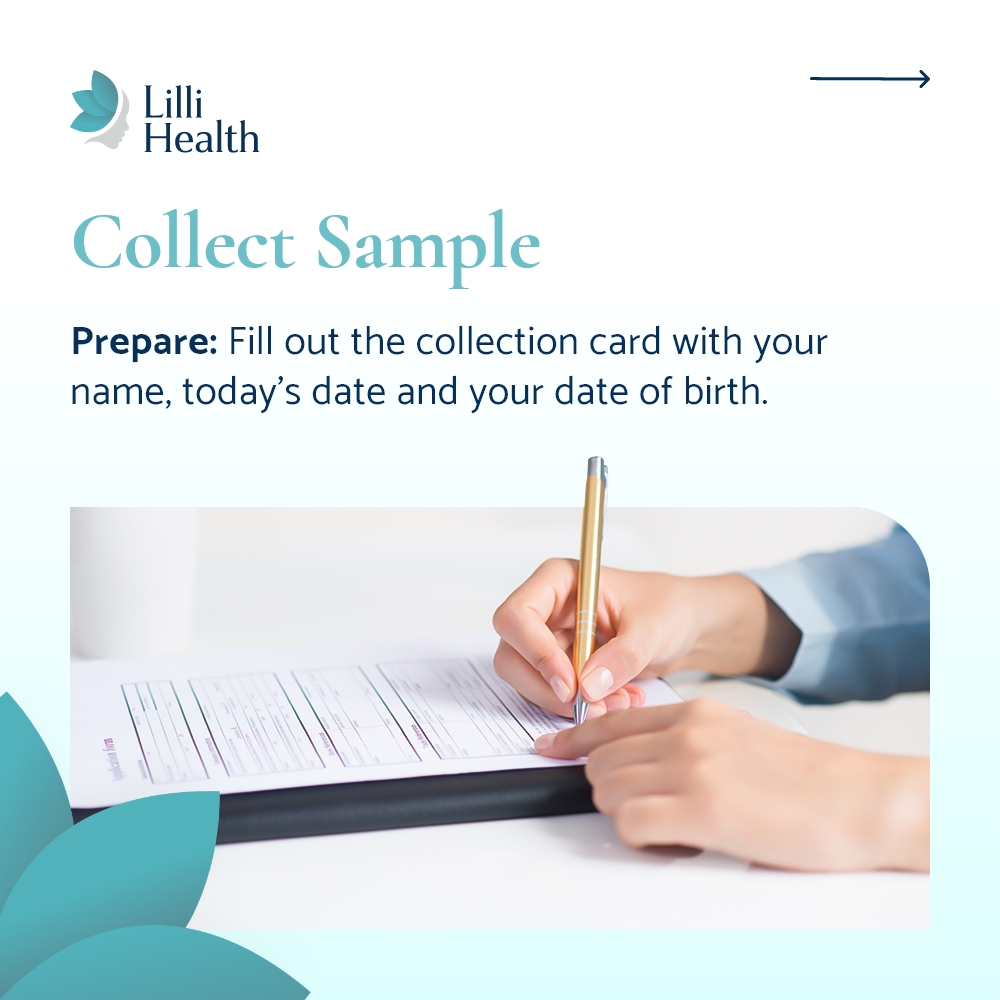
- Ask your healthcare provider to check your fasting insulin and 2-hour insulin levels
Sitting in a lab for two hours to get your 2-hour insulin test might be annoying—but not nearly as annoying as going through multiple rounds of IVF. Promise.
Bottom Line
Fertility isn’t just about your reproductive organs—it’s about your whole system. And insulin touches every part of it. Whether you’re just getting started or gearing up for round 2 (or 5) of IVF, make this your foundation: lower insulin, balance hormones, support implantation, and set the stage for a healthy pregnancy.
It’s not just about getting pregnant—it’s about staying pregnant, thriving during pregnancy, and supporting your (and your baby’s) long-term health too.
And if your doctor isn’t talking about insulin? You’re already one step ahead.
Bottom Line
Luo Z, et al. Impact of Insulin Resistance on Ovarian Sensitivity and Pregnancy Outcomes in Patients with Polycystic Ovary Syndrome Undergoing IVF. J Clin Med. 2023. Read more
Yang T, et al. Homeostatic Model Assessment for Insulin Resistance Is Associated With Late Miscarriage in Non-Dyslipidemic Women Undergoing Fresh IVF/ICSI Embryo Transfer. Front Endocrinol (Lausanne). 2022. Read more
Vega M, et al. Direct toxicity of insulin on the human placenta and protection by metformin. Fertil Steril. 2019. Read more
Chen Y, et al. Insulin Resistance is a Risk Factor for Early Miscarriage and Macrosomia in Patients With Polycystic Ovary Syndrome From the First Embryo Transfer Cycle: A Retrospective Cohort Study. Front Endocrinol (Lausanne). 2022. Read more