What to Do After Your PCOS Diagnosis
Getting diagnosed with PCOS can feel overwhelming. You may have been struggling with symptoms like irregular cycles, acne, hair loss, weight gain, or infertility for years without knowing the cause. Now that you have a diagnosis, you might be wondering—what next?
PCOS is a complex condition affecting up to 1 in 5 reproductive-aged women, but the good news is that there are effective ways to manage it and take control of your health. Here’s what to do after your PCOS diagnosis to start feeling better and improving your long-term well-being.
1. Understand What PCOS Really Is
PCOS is often described as a “hormonal imbalance,” but at its core, it is a metabolic condition driven by insulin resistance. In fact, 70-95% of people with PCOS have some degree of insulin resistance, even if they are not overweight.
High insulin levels trigger excess androgen production, which leads to many of the classic PCOS symptoms, including:
- Irregular or missing periods
- Acne and oily skin
- Hair thinning or hair loss
- Excess facial or body hair growth
- Unexplained weight gain or difficulty losing weight
- Fatigue and brain fog
- Fertility challenges
- Sleep problems
- Mood swings
- Anxiety and depression
The key to managing PCOS is not just treating symptoms—it is addressing insulin resistance first.
2. Get the Right Lab Tests
Many doctors focus only on hormone levels when diagnosing PCOS, but because insulin resistance is the root cause for most people, it is critical to test insulin levels.
Ask your doctor for:
- Fasting insulin – A high level suggests insulin resistance.
- 2-hour insulin after a glucose tolerance test – Many people with PCOS have normal fasting insulin but elevated insulin after eating.
- Hemoglobin A1C and fasting glucose – These measure long-term and current blood sugar levels but do not reveal insulin resistance.
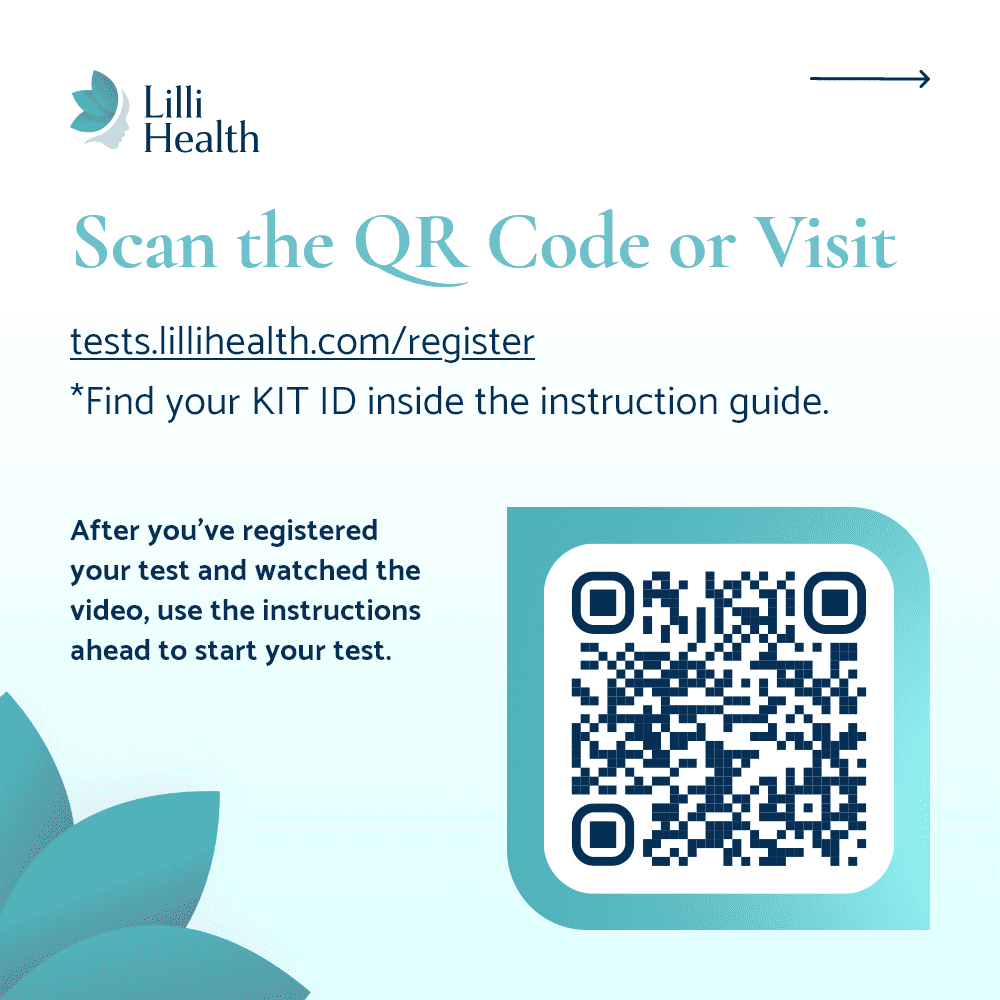
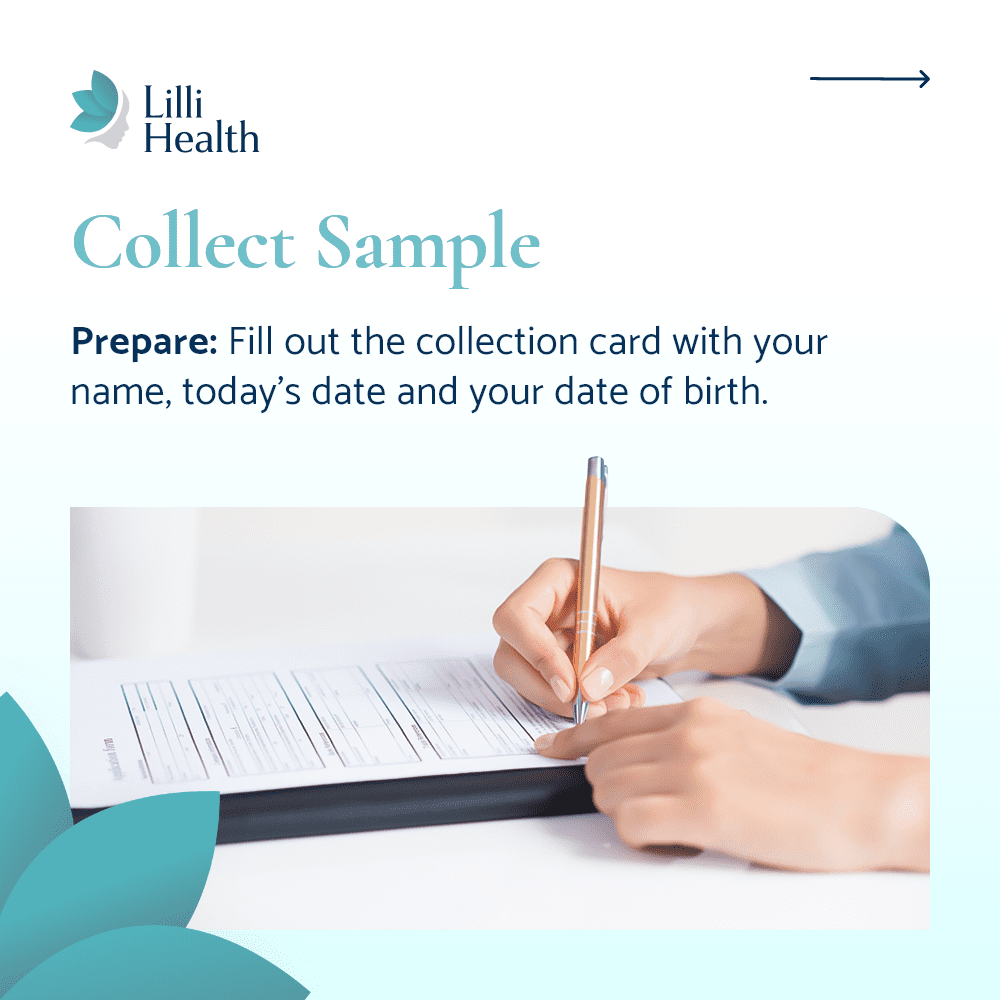
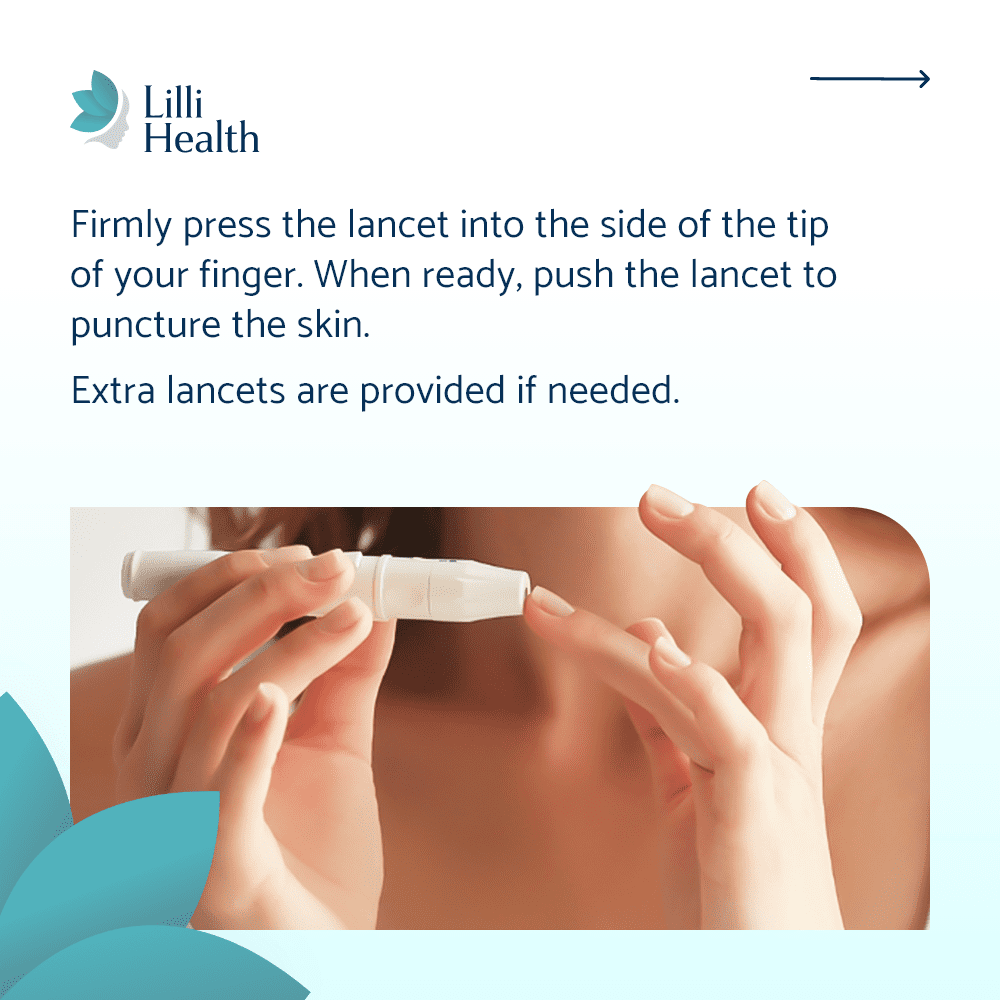
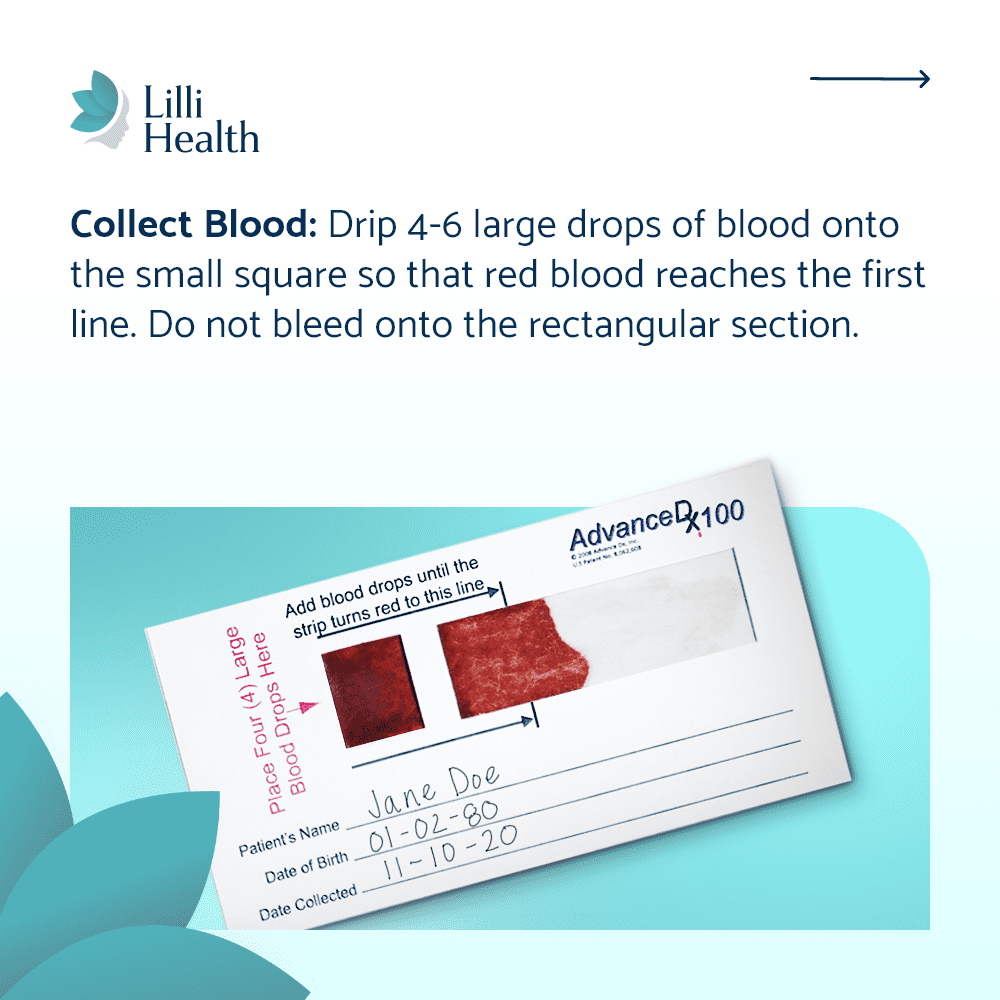
Testing insulin levels early helps you take action before insulin resistance progresses to prediabetes or type 2 diabetes. If your doctor does not offer insulin testing, you can check your levels at home with Lilli Metabolic Testing Kits.
3. Make an Insulin-First Lifestyle Shift
Most traditional PCOS treatments focus on symptom management rather than the root cause. Birth control, metformin, and other medications can sometimes help, but focusing on lowering insulin is the most effective long-term strategy.
A Low Insulin Lifestyle is the only approach that directly targets insulin resistance. Instead of focusing on weight loss, calorie counting, or restrictive eating, it prioritizes:
- Non-starchy vegetables and whole fruits instead of grains, beans, and potatoes
- Healthy fats like avocado, olive oil, and nuts to keep insulin low
- Moderate protein to prevent excessive insulin release from animal-based foods
- Fermented dairy instead of regular dairy since milk and whey protein spike insulin
This approach supports hormone balance, regulates cycles, improves fertility, and restores metabolic health naturally.
4. Manage Stress and Prioritize Sleep
Stress and sleep directly affect insulin levels and hormone balance. Chronic stress increases cortisol, which raises insulin and worsens PCOS symptoms. Poor sleep can also lead to higher insulin levels, increased cravings, and more fatigue.
- Reduce stress with deep breathing, meditation, or time outdoors
- Aim for at least 7-8 hours of quality sleep each night
- Avoid late-night eating to keep insulin low overnight
5. Find a PCOS-Savvy Doctor
Many doctors still treat PCOS as just a reproductive condition and may not focus on insulin resistance. If your doctor is not testing insulin or dismissing your concerns, consider finding one who understands the metabolic side of PCOS.
Functional medicine doctors, endocrinologists, and some OB-GYNs specializing in PCOS are more likely to take a comprehensive approach rather than just prescribing birth control or metformin without addressing the underlying metabolic issues.
6. Track Your Progress and Stay Empowered
PCOS management is a journey, but the most important thing is knowing that you have control.
- Track your insulin levels every few months to monitor improvements
- Pay attention to symptoms—regulated cycles, clearer skin, and stable energy are signs that your approach is working
- Stay consistent—long-term changes yield the best results
The Bottom Line
A PCOS diagnosis can feel overwhelming, but you are not powerless. By addressing insulin resistance, making targeted lifestyle changes, and tracking your progress, you can take control of your health and feel your best.
If you are unsure where to start, testing your insulin levels is the first step. With Lilli At-Home Insulin Testing Kits, you can measure your metabolic health from home and get a clearer picture of what to do next.