Blood Glucose vs. Insulin: What’s the Difference?
There’s a lot of focus on blood sugar these days. From continuous glucose monitors (CGMs) to A1c tests, many people think that as long as their blood sugar is normal, they are in the clear. But what if I told you that blood sugar only tells part of the story?
The real issue often starts long before blood sugar ever becomes a problem—high insulin levels. Insulin can be hire for decades before blood sugar starts to rise, and by the time most people are diagnosed with type 2 diabetes, insulin has been high for years, quietly wreaking havoc on the body.
Let’s break down the difference between blood glucose and insulin and why testing insulin levels is just as—if not more—important.
The Role of Blood Glucose
Blood glucose, or blood sugar, refers to the amount of sugar circulating in your bloodstream. Your body tightly regulates blood glucose because too much can be toxic, damaging organs, blood vessels, and nerves over time.
When you eat, especially carbohydrates, your blood sugar rises. In response, your pancreas releases insulin to shuttle glucose out of the bloodstream and into cells, where it can be used for energy or stored as fat. Once glucose is cleared, blood sugar returns to normal.
Doctors often rely on blood sugar tests, like fasting glucose or A1c, to assess metabolic health. However, these tests only show when blood sugar has already become a problem. By that point, insulin resistance has usually been present for years.
What Is Insulin?
Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. Think of it as the key that unlocks your cells so glucose can enter and be used for energy. Without insulin, glucose would stay in your bloodstream instead of getting into your cells where it’s needed.
However, insulin isn’t just about lowering blood sugar—it’s also a storage hormone. When insulin is high, it tells your body to store excess energy as fat. It also affects other hormones, including testosterone, estrogen, and cortisol, making it a major player in overall health.
Insulin levels can be measured with:
- Fasting insulin test – Measures how much insulin is in your blood after fasting for at least 8 hours. A healthy fasting insulin level is typically between 3-8 mIU/mL.
- 2-hour insulin test – Measures how much insulin your body produces in response to eating. This is useful for detecting early insulin resistance, though it is rarely ordered in standard medical practice.
- HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) – A calculation that estimates insulin resistance using fasting insulin and fasting glucose levels.
- C-Peptide Test – When your pancreas produces insulin, it also releases an equal amount of C-peptide. Since insulin gets cleared from the blood quickly, while C-peptide sticks around longer, testing C-peptide can provide a clearer picture of how much insulin your pancreas is making.
The problem? Insulin resistance develops long before blood sugar levels start to rise, meaning you can have high insulin levels for years before any changes show up in a blood sugar test.
How Blood Glucose and Insulin Work Together
Blood glucose and insulin work in a feedback loop to keep metabolism functioning properly. Here’s what should happen in a healthy system:
- You eat a meal that contains carbohydrates.
- Your blood sugar rises as glucose enters your bloodstream.
- Your pancreas releases insulin to help shuttle glucose into your cells.
- Blood sugar levels return to normal, and insulin levels drop.
In someone with insulin resistance, the process doesn’t work as smoothly:
- The cells stop responding to insulin properly.
- The pancreas produces more insulin to force glucose into the cells.
- Insulin levels stay high, even when blood sugar appears normal.
- Over time, the pancreas can’t keep up, leading to elevated blood sugar and eventually type 2 diabetes.
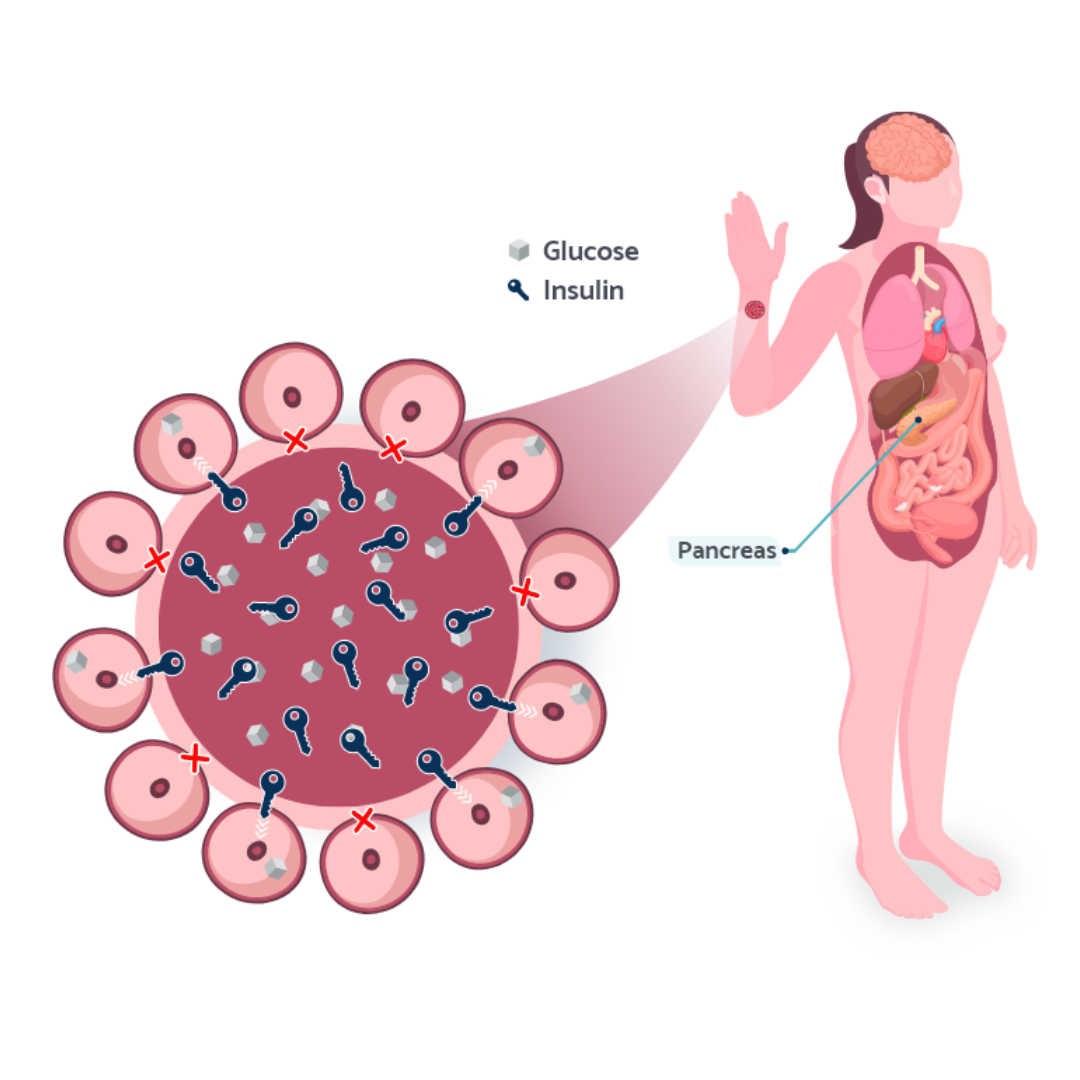
If you see the image above, the (X) marks the cells that no longer respond to insulin appropriately, which is why there is more insulin in the blood relative to glucose. This is why relying on blood sugar tests alone can be misleading. You might have normal glucose levels while your insulin has been sky-high for years, driving weight gain, cravings, inflammation, and hormone imbalances without you even knowing it.
Why High Insulin Matters (Even If Blood Sugar Is Normal)
Most healthcare providers focus on blood sugar when assessing metabolic health, but high insulin levels can be a warning sign of trouble long before blood sugar rises. Here’s why high insulin matters:
- Weight gain and difficulty losing weight – Insulin is a fat-storage hormone. High insulin levels make it nearly impossible to burn stored fat for energy.
- Increased hunger and cravings – High insulin drives blood sugar crashes, making you feel constantly hungry and craving carbs.
- PCOS and hormone imbalances – High insulin triggers excess testosterone production, contributing to irregular cycles, acne, and infertility in women with PCOS.
- Inflammation and chronic disease – High insulin is linked to heart disease, Alzheimer’s, cancer, and metabolic disorders.
- Fatigue and brain fog – Insulin resistance disrupts energy metabolism, leading to sluggishness and difficulty concentrating.
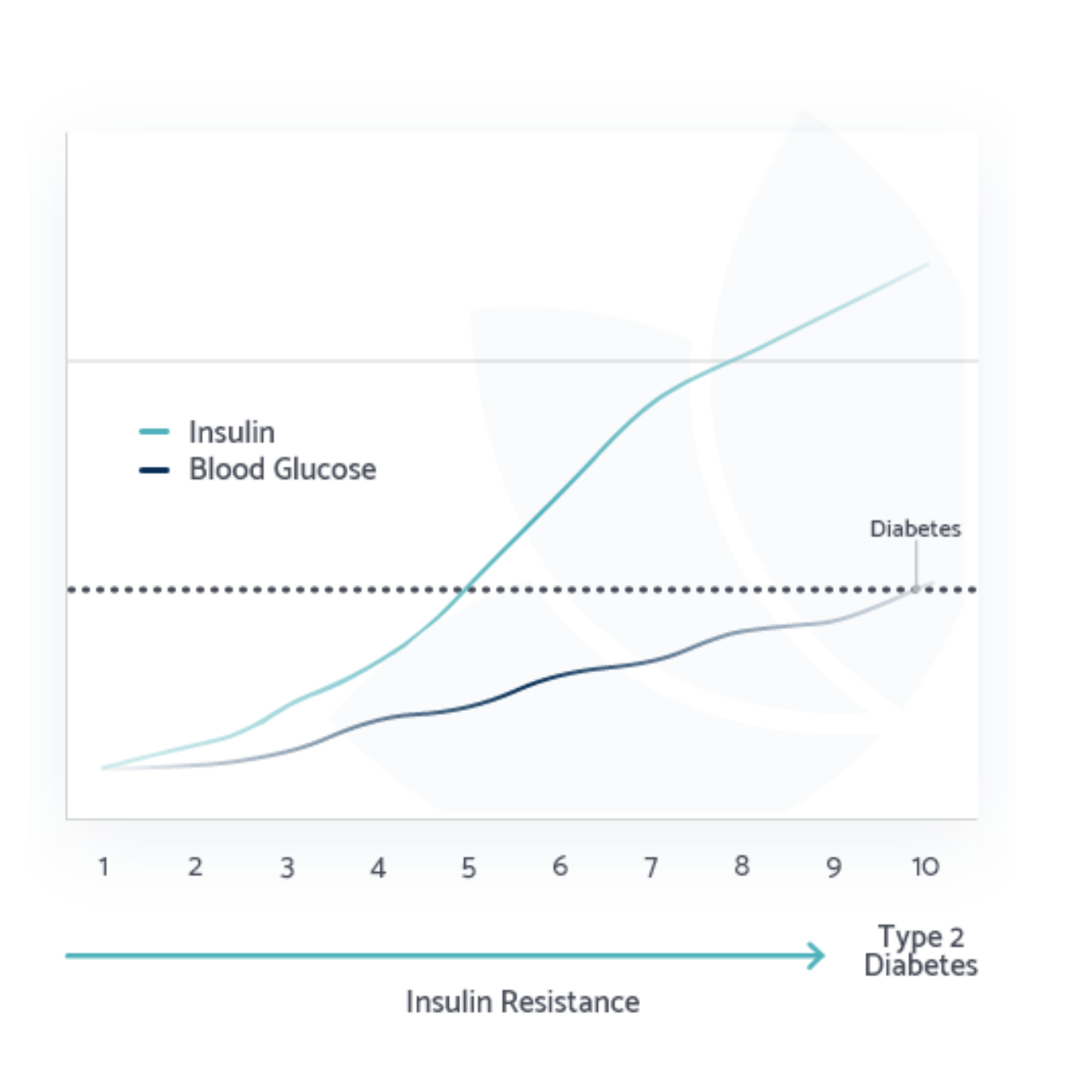
By the time high blood sugar shows up on a test, insulin has often been elevated for years, silently driving these issues. Check out this graph. It illustrates what typically happens when you only test blood glucose without measuring insulin.
This graph shows what you would likely see if you tested most adults’ blood sugar (navy) and insulin (turquoise) levels over time. The navy blue line represents blood sugar, which remains normal for years, while the turquoise line shows insulin levels creeping up over time.
You could even think of this in decades. In your 20s or 30s, insulin may already be higher than normal, but your blood sugar looks fine, so you get a clean bill of health. By your 40s or 50s, insulin levels are significantly elevated, but unless your doctor tests for insulin, no one knows. Then, in your 50s or 60s, your pancreas can’t keep up, blood sugar finally rises, and you’re diagnosed with type 2 diabetes.
By the time most people are diagnosed, they’ve had insulin resistance for decades. And high insulin levels aren’t just linked to diabetes—they’re associated with heart disease, Alzheimer’s, PCOS, infertility, and even cancer.
Why You Should Test Insulin, Not Just Blood Sugar
Most doctors don’t test insulin. Instead, they focus on blood sugar and A1c, which can remain normal for years before revealing a problem. This is why many people with insulin resistance go undiagnosed for decades.
To catch metabolic issues early, get your insulin tested. Ideally, fasting insulin should be between below 8 mIU/mL and 2hr insulin should be below 50 mIU/mL. Anything higher suggests insulin resistance, even if your blood sugar is normal.
Other markers, like C-peptide, TG/HDL ratio, and inflammatory markers like CRP, can also provide insight into your metabolic health.
CGMs are popular right now, but they only measure blood sugar, not insulin. Your CGM graph might look perfect, but that doesn’t mean your metabolism is healthy. Your pancreas could be flooding your system with insulin to keep that line steady, masking insulin resistance in the background. If you want the full picture, testing insulin, not just blood sugar, is the key to understanding and improving your long-term health.
The Bottom Line
Blood sugar and insulin are not the same, and relying solely on blood sugar tests can leave you in the dark about your metabolic health. If you want to truly understand your body’s metabolism and prevent long-term health issues, testing insulin is key.
By following a Low Insulin Lifestyle, you can keep insulin levels in check, reverse insulin resistance, and reduce the risk of metabolic diseases before they develop. Don’t wait until blood sugar becomes a problem—take action now.
References
Zhang AMY, Wellberg EA, Kopp JL, Johnson JD. Hyperinsulinemia in obesity, inflammation, and cancer. Diabetes Metab J. 2021. Read more
Templeman NM, Skovsø S, Page MM, Lim GE, Johnson JD. A causal role for hyperinsulinemia in obesity. Journal of Endocrinology. 2017. Read more
Thomas DD, Corkey BE, Istfan NW, Apovian CM. Hyperinsulinemia: An early indicator of metabolic dysfunction. J Endocr Soc. 2019. Read more
Johnson JL, Duick DS, Chui MA, Aldasouqi SA. Identifying Prediabetes Using Fasting Insulin Levels. Endocrine Practice. 2010. Read more