The METABOLIC Study: Unlocking the Body’s Ability to Burn Fat
After the PILOT study demonstrated how lowering insulin could improve PCOS symptoms and restore fertility, the next big question was:
What is insulin actually doing to metabolism, and why does it make it so hard for people with PCOS to burn fat?
That’s where the METABOLIC Study came in.
For years, people with PCOS had been told that their inability to lose weight was because they ate too much or didn’t exercise enough. But that explanation didn’t hold up. Even women who followed traditional low-calorie diets struggled to lose weight, and when they did, they often gained it all back (or more).
So what if the real problem wasn’t calories—but insulin?
This study set out to measure exactly what was happening in the metabolism of women with PCOS before and after following a Low Insulin Lifestyle.
Why High Insulin Prevents Fat Burning
Insulin isn’t just a blood sugar hormone—it’s also the master regulator of fat storage and fat burning.
When insulin is high, the body is in fat-storage mode—it holds onto fat and prevents stored fat from being used for energy. This means that even when someone fasts overnight, their body still isn’t burning fat efficiently. Normally, when you go several hours without eating (like overnight while you sleep), your body should switch to burning stored fat for energy. This is what happens in a healthy metabolism.
However, in women with PCOS, this wasn’t happening.
To measure this, we looked at a key metabolic marker called the Respiratory Exchange Ratio (RER).
What Is Respiratory Exchange Ratio (RER)?
RER is a scientific measurement of what fuel your body is burning—carbohydrates or fat. It is measured by looking at how much oxygen you breathe in versus how much carbon dioxide you exhale. Science is so cool.
- RER of 1.0 or higher: Your body is burning mostly carbohydrates (typical in patients with insulin resistance)
- RER of 0.85: Your body is using a mix of carbs and fats
- RER of 0.7: Your body is burning mostly fat (this is ideal for weight loss and metabolic flexibility)
In healthy individuals, RER naturally drops overnight as the body shifts into fat-burning mode during fasting. However, in women with PCOS, we found something alarming:
Even after fasting all night, their bodies were still burning sugar, not fat!!
This confirmed what we suspected: high insulin levels were blocking fat burning.
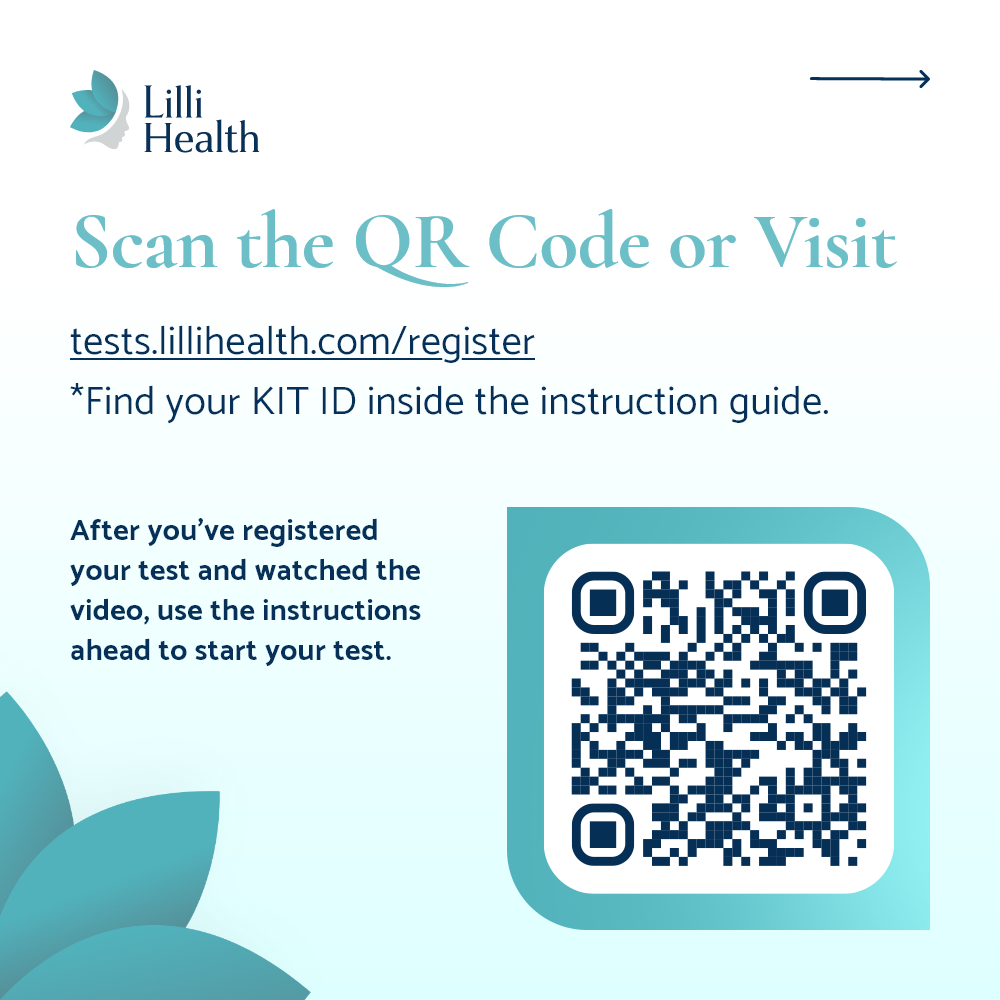
How We Tested Fat Metabolism
To see whether we could improve fat oxidation, we had participants:
- Drink a high-fat shake
- Measure how their body responded for five hours
Before the study, their bodies were only burning the sugar in the shake and storing all the fat as body fat.
But after following a Low Insulin Lifestyle for eight weeks, we measured them again.
This time, something incredible happened. For the first time, they were able to access their own fat stores for energy—a crucial step for sustainable weight loss.
The Results: Turning the Body Into a Fat-Burning Machine
After just eight weeks, we saw:
- A HUGE improvement in fat burning—their bodies were now actually burning the fat in the shake for energy instead of storing it.
- No metabolic slowdown. Even though their total energy expenditure slightly declined (as expected when your body weighs less), when we measured energy burned per pound of body weight, it didn’t decrease at all. This is completely different from what happens on traditional low-calorie diets.
- No muscle loss. Despite losing weight, participants maintained their lean muscle mass—even though they were not allowed to exercise during the study.
This is exactly the opposite of what happens on restrictive diets, where metabolism slows down and people often lose muscle along with fat.
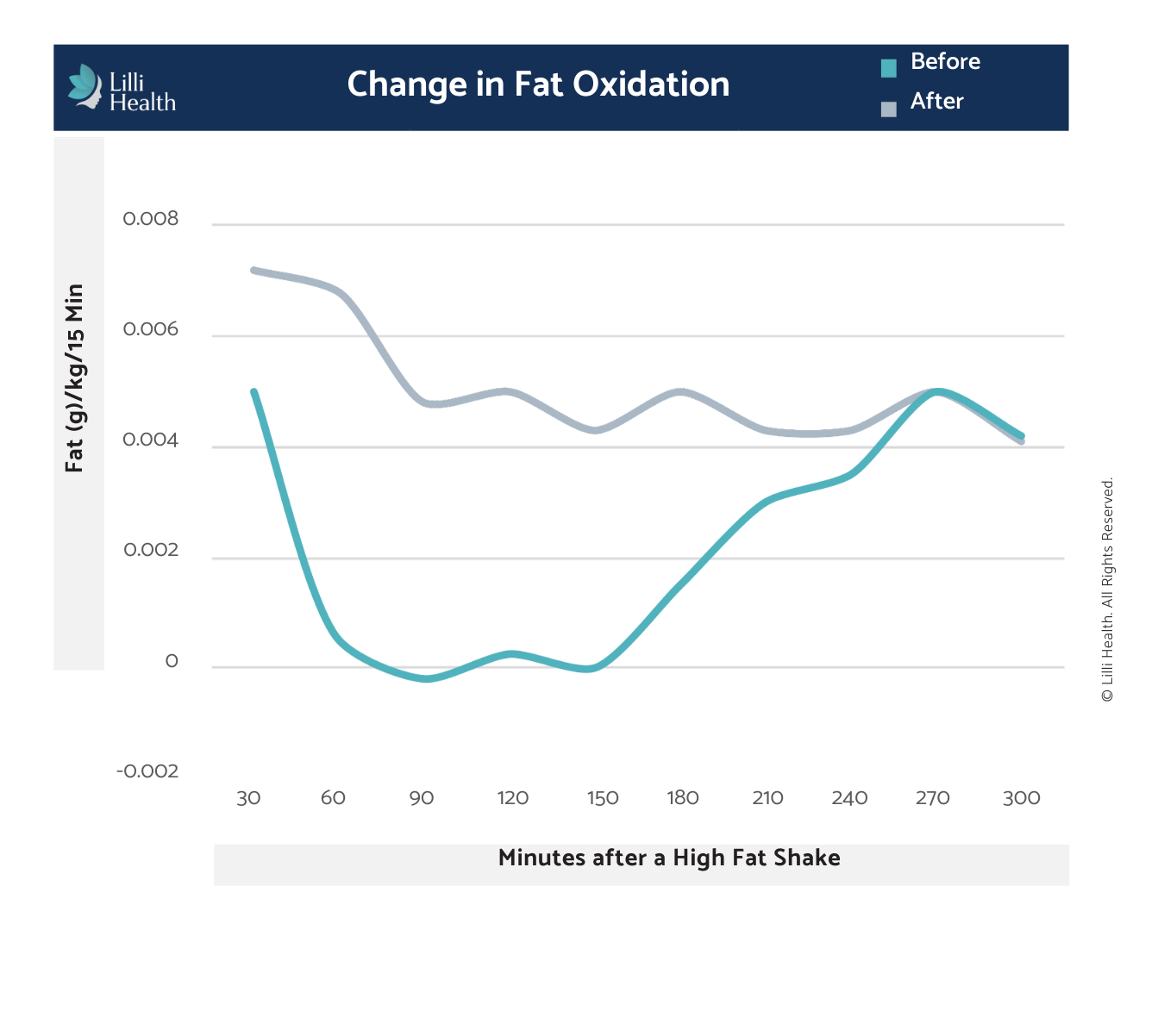
This graph shows how the body’s ability to burn fat changed before and after following a Low Insulin Lifestyle. Before (blue line), participants’ bodies barely burned any fat after drinking a high-fat shake—instead, they were stuck burning sugar and storing the fat. After just eight weeks on this lifestyle (gray line), their bodies became much better at using fat for energy. This means lowering insulin helps unlock fat burning, making weight loss easier and more sustainable without extreme dieting or muscle loss.
Why This Study Was a Game-Changer
The METABOLIC Study proved that:
- High insulin levels prevent fat burning in women with PCOS.
- Lowering insulin allows the body to naturally burn fat instead of storing it.
- Unlike traditional dieting, this approach doesn’t slow metabolism or cause muscle loss.
This study completely changed the narrative around PCOS and weight loss. It showed that PCOS isn’t a “calories in, calories out” problem—it’s an insulin problem.
This study paved the way for further research and proved that the Low Insulin Lifestyle is the key to reversing insulin resistance, improving metabolism, and achieving long-term health without metabolic damage.
Why Participants Didn’t Lose Muscle (Even Without Exercise)
Another major benefit? Patients didn’t lose muscle mass—even though they weren’t exercising.
This is a huge deal.
Why? Lower insulin meant they could finally burn stored fat for fuel meaning their bodies didn’t need to burn muscle for energy.
What This Means for Women with PCOS
The METABOLIC study showed that insulin resistance in PCOS isn’t just about weight—it fundamentally blocks your ability to burn fat.
But it also proved that this can be reversed.
By lowering insulin through a Low Insulin Lifestyle, participants were able to:
- Start burning fat for efficiently
- Maintain muscle mass and metabolism
- Avoid metabolic slowdown seen with other diets
This laid the foundation for what happened next.
The Next Step: The Case Series
Now that we saw how insulin was blocking fat burning, we wanted to see what happened when real-world patients followed a Low Insulin Lifestyle for fertility.
That’s where the Case Series comes in. This study took women with PCOS who had been struggling with infertility who conceived naturally after following a Low Insulin Lifestyle.
This was the real-world proof that lowering insulin isn’t just about weight—it’s about restoring overall health.
References
Pohlmeier AM, et al. Effect of a low-starch/low-dairy diet on fat oxidation in overweight and obese women with polycystic ovary syndrome. Appl Physiol Nutr Metab. 2014. Read more