The PILOT Study: The Beginning of a Groundbreaking Discovery
The PILOT study was where it all started. After discovering the power of insulin in my own health journey, I knew I needed to take this to research. But getting funding as a doctoral student isn’t easy. That’s why receiving a prestigious research grant from the Laura W. Bush Institute for Women’s Health was such a big deal—it meant that this question was worth exploring at a higher level.
A PILOT study is a small-scale preliminary study conducted before a larger trial to test whether an approach is effective, feasible, and worth studying on a bigger scale. It helps researchers refine their methods and determine if their hypothesis holds up. This study was a first step in proving that insulin—not calories—was the key driver of PCOS symptoms.
With this funding, we were able to recruit 24 patients diagnosed with PCOS to follow what would later become known as the Low Insulin Lifestyle.
But what happened next was unexpected.
The Unexpected Results
Before the study could even be completed, several participants dropped out—because they got pregnant naturally. For many of these women, they had been told they would never conceive without fertility treatments. And yet, within a matter of weeks, they were ovulating on their own.
This was a major lightbulb moment. If lowering insulin could restore ovulation this quickly, what else could it do?
Study Design: What Did We Test?
The 24 participants in the study were instructed to follow a Low Insulin Lifestyle for eight weeks.
This meant:
- No calorie restriction—they were allowed to eat as much as they wanted
- Focusing on foods that keep insulin low (avoiding starch, sugar, and non-fermented dairy)
- Eating naturally satisfying meals—without measuring portions or tracking macros
Although they weren’t told to count calories or macros, when we analyzed their food intake, we found that on average, participants were naturally eating:
- ~1,500 calories per day
- ~70g of fat, mostly from monounsaturated fats (think avocados, olive oil, nuts, and seeds)
- ~25g of fiber per day
- ~90g of carbohydrates
As you can see from what their food logs showed, they weren’t eating low-carb or keto, they weren’t overloading on protein. They just ate real food. This wasn’t a diet—it was a metabolic reset.
The Results: What We Found
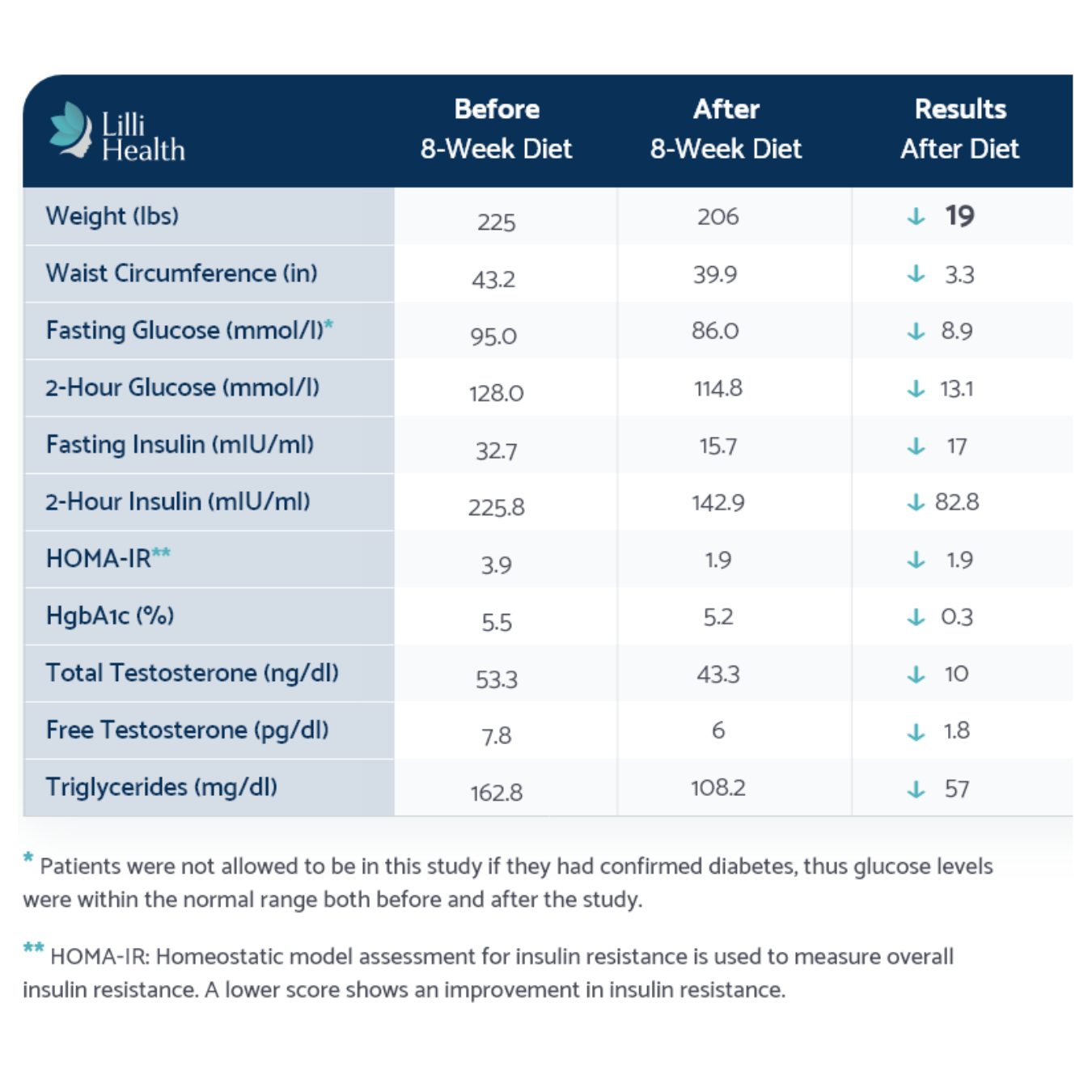
At the end of eight weeks, the results spoke for themselves:
- Fasting and 2-hour insulin levels dropped significantly—even in those who had “normal” blood sugar’
- A1c levels were significantly improved, even though they started out relatively normal
- Weight loss occurred naturally without calorie restriction (19 POUNDS!) and patients lots inches around their waist and hips
- Menstrual cycles regulated, and several patients conceived during the study
- Patients reported improved PCOS symptoms
- Markers of inflammation and cardiovascular risk improved
Can we take a moment to acknowledge that every single patient in this study had completely normal glucose and A1c levels, yet their insulin levels were 4x higher than they should have been? And yet, insulin testing still isn’t part of clinical guidelines. So basically, all of these patients would have been given a clean bill of health, a pat on the back, and told to “just keep trying”—all while their actual problem was being completely ignored.
What This Means for PCOS and Insulin Resistance
Even in a small sample, this study demonstrated that insulin is a key driver of PCOS symptoms. And more importantly, lowering insulin can lead to rapid, meaningful improvements in metabolic health, ovulation, and overall well-being.
This study paved the way for our next research study: The METABOLIC Study, which would take these findings even further.
References
Phy JL, et al. Low Starch/Low Dairy Diet Results in Successful Treatment of Obesity and Co-Morbidities Linked to Polycystic Ovary Syndrome (PCOS). J Obes Weight Loss Ther. 2015. Read more