The Science Behind This Lifestyle and the Research That Supports It
This lifestyle wasn’t developed in a lab or as a trendy diet—it was born out of personal struggle. I developed this way of eating when I was in a dark place, desperately trying to figure out what was wrong with my body. Even as a dietitian, doing everything I was taught—counting calories, eating whole grains, and following all the conventional nutrition advice—nothing worked. In fact, I was only getting worse.
It started with a question: What is driving this? How can I fix it?
So, I started reading. And I didn’t stop. This was in 2009—before Instagram influencers and TikTok experts. I dove into PubMed, reading every research paper I could find. I came across something that wasn’t being talked about back then: insulin.
At the time, I had learned nothing about PCOS—especially not the role of insulin. In school, PCOS was briefly mentioned during a discussion about type 2 diabetes. That’s it. But the more I read, the more I realized that PCOS is fundamentally a metabolic disorder driven by insulin.
Then I asked myself, what drives insulin? Because all I had learned in school about insulin was how much to give a diabetic to manage blood glucose. Nothing about what causes insulin levels to rise or how to lower them. That was the moment everything changed.
I began experimenting on myself, changing how I ate—not by focusing on calories, carbs, or portion control—but by prioritizing foods that didn’t spike insulin. And it worked. For the first time, my symptoms improved, my cycles regulated, and I felt like myself again.
Then I wondered… If this worked so well for me, would it work for others?
The rest is history.
I received a prestigious Laura W. Bush Institute for Women’s Health Research grant—an incredible achievement for a doctoral student—and officially began studying the effects of a Low Insulin Lifestyle. I partnered with a reproductive endocrinologist and PCOS expert to conduct the first study, and the results were even more powerful than I could have imagined.
That was over a decade ago. Today, I’m still conducting research, refining this approach, and proving again and again that an insulin-first approach is the key to reversing metabolic dysfunction.
An Overview of the Research
Over the years, we’ve conducted multiple studies on the Low Insulin Lifestyle, each providing more evidence that focusing on insulin, not calories, is the key to long-term metabolic health.
The Pilot Study
Our first study was small but incredibly promising. We had participants follow the Low Insulin Lifestyle for just 8 weeks. On average, participants:
- Lost 19 pounds
- Dropped fasting insulin by over 50%
- Experienced significant symptom relief (better cycles, improved energy, less hunger)
Even more impressive? This was without calorie restriction—just by eating foods that naturally kept insulin levels low.
The Metabolic Study
This study went deeper into fat metabolism and showed that lowering insulin drastically improves fat oxidation—meaning that instead of storing fat, the body actually burns it for fuel.
Participants following the Low Insulin Lifestyle:
- Better able to burn fat
- Showed improved metabolic flexibility (the ability to switch between burning carbs and fat efficiently)
- Had significantly lower insulin levels and inflammation markers
The Case Series
A group of real-world patients who had been struggling with infertility followed a Low Insulin Lifestyle and were tracked by an independent group of fertility specialists and Ob/Gyns. The results were remarkable:
- Patients conceived naturally within an average of 86 days after starting this lifestyle
This case series further reinforces what we’ve seen in clinical studies—improving ovulation and increasing the chances of pregnancy start with lowering insulin. We’ve known this for a long time, but generally, it’s just treated using metformin. By addressing insulin resistance through a Low Insulin Lifestyle, the body can restore hormonal balance, supporting natural conception without the need for intensive fertility treatments.
The Randomized Controlled Trial (RCT)
This was the gold standard of research—a randomized controlled trial comparing the Low Insulin Lifestyle to conventional dietary advice (“eat less and exercise more”) plus metformin. This study was conducted by an independent group of reproductive endocrinologists and Ob/Gyns. The results were undeniable:
- A Low Insulin Lifestyle was significantly more effective at reducing insulin and A1c than standard lifestyle advice and treatment
- Participants lost more weight without calorie restriction
- Markers of inflammation and cardiovascular health improved
Ongoing Research: The DAISY and LILACS Studies
We are continuing to study the long-term effects of a Low Insulin Lifestyle and how it impacts metabolic health, hormone balance, and overall well-being.
The DAISY Study
DAISY: Determining Associations of Insulin Resistance with Symptoms in PCOS Patients
- Measuring insulin resistance in patients with PCOS
- Exploring correlations between insulin levels, medical history, and symptoms
- Providing more evidence that insulin testing should become a standard part of PCOS diagnosis and treatment
Study Link: DAISY Study – Clinical Trials
The LILACS Study
This is our most exciting study yet—the LILACS study is investigating the Low Insulin Lifestyle as an FDA-cleared treatment for weight loss in patients with PCOS.
- A randomized controlled trial to test the effectiveness of the Lilli App and Low Insulin Lifestyle
- Designed to support FDA clearance of the first-ever digital therapeutic for insulin resistance and PCOS
- If successful, this could change the standard of care for PCOS and metabolic health
The Bottom Line
This lifestyle is not just another diet. It’s not about counting carbs, calories, points, or macros. It’s about understanding insulin and making intentional choices that work with your metabolism, not against it.
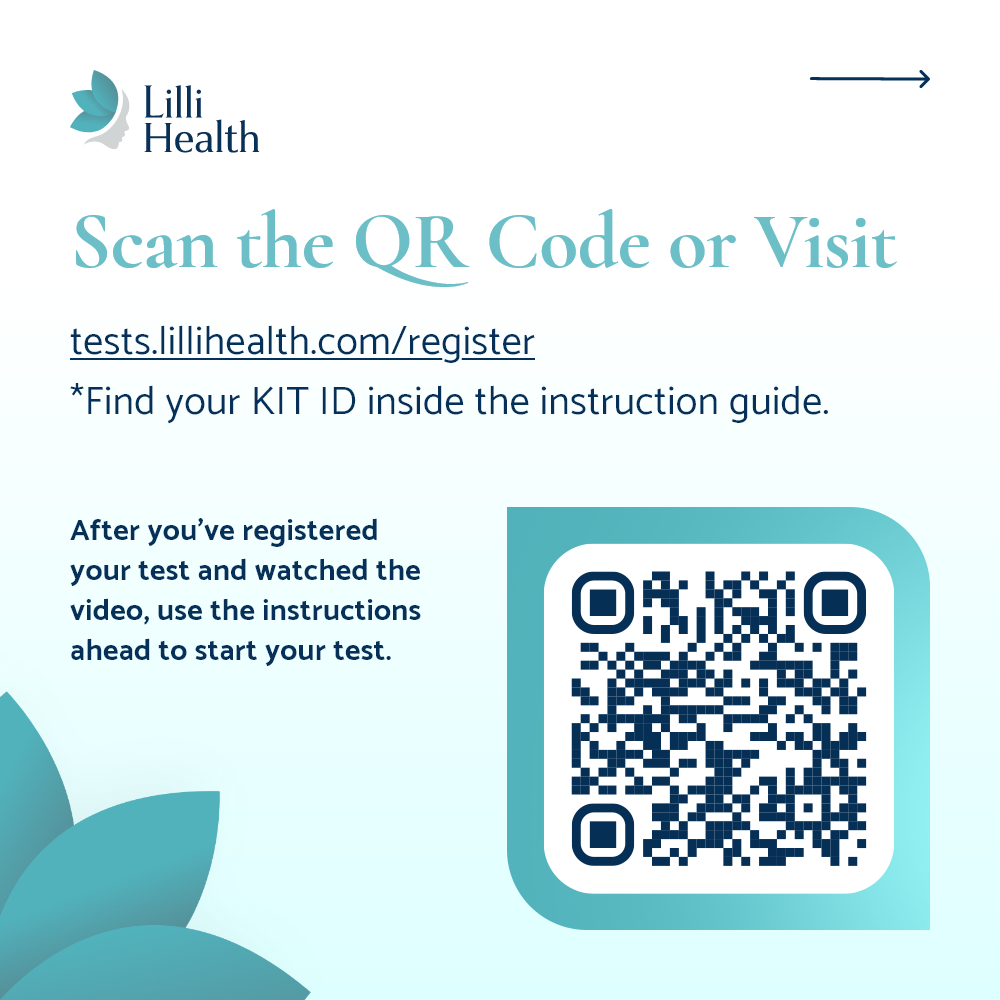
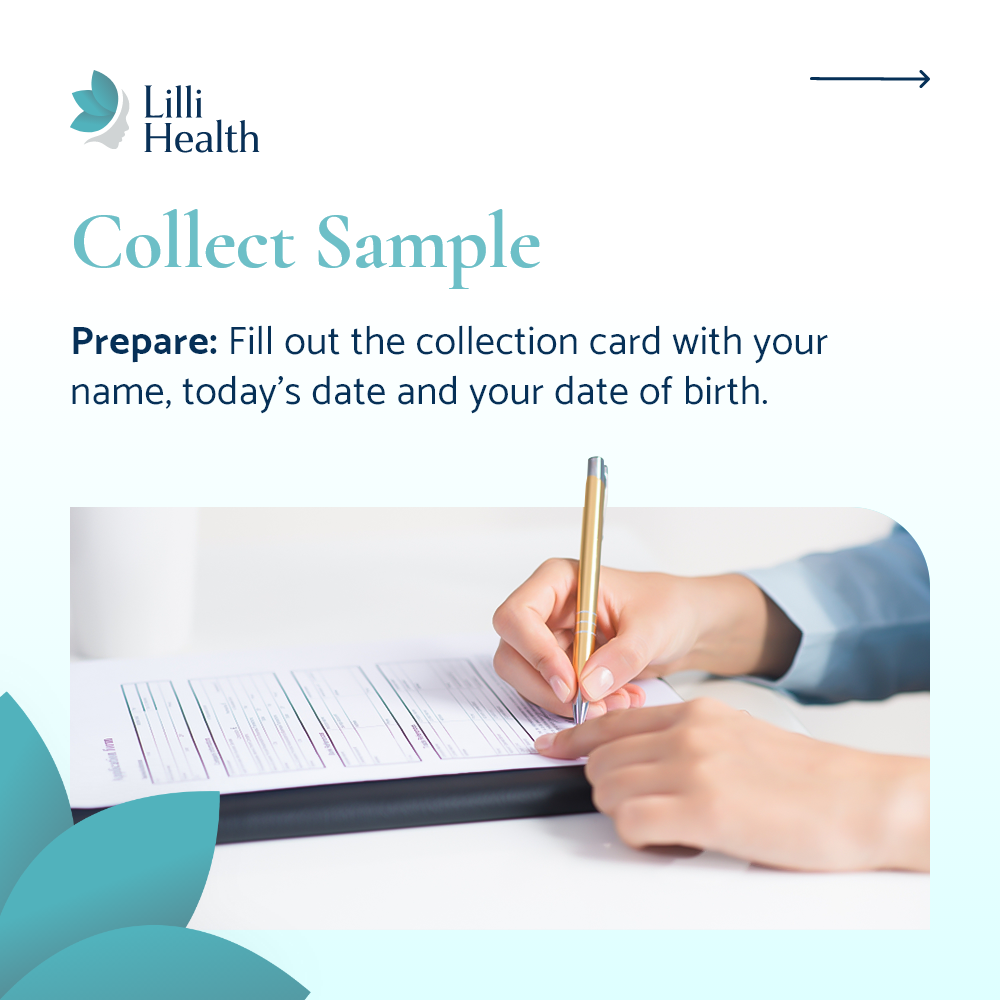
The research speaks for itself. This works. And now, for the first time, we have the technology (through the Lilli App and Lilli Metabolic Testing Kits) to track and measure metabolic health like never before.
This is the easiest, most sustainable way to lower insulin, reverse insulin resistance, and live a healthier life.
And we’re just getting started.
References
- Pohlmeier AM, et al. Effect of a low-starch/low-dairy diet on fat oxidation in overweight and obese women with polycystic ovary syndrome. Appl Physiol Nutr Metab. 2014. Read more
- Phy JL, et al. Low Starch/Low Dairy Diet Results in Successful Treatment of Obesity and Co-Morbidities Linked to Polycystic Ovary Syndrome (PCOS). J Obes Weight Loss Ther. 2015. Read more
- Kishan R, et al. Spontaneous Pregnancies in Polycystic Ovary Syndrome (PCOS) Patients with a Low Starch/Low Dairy Diet: A Retrospective Case Series. J Community Med Public Health. 2022. Read more
- Jackson B, et al. Nutritional education (face-to-face and video instruction) for polycystic ovary syndrome results in greater reduction in bmi and hemoglobin a1c than caloric restriction, exercise and metformin (Abstract). Fertility and Sterility. 2022. Read more
- Rastad H, et al. Dairy consumption and its association with anthropometric measurements, blood glucose status, insulin levels, and testosterone levels in women with polycystic ovary syndrome: a comprehensive systematic review and meta-analysis. Front Endocrinol (Lausanne). 2024. Read more