PCOS is often associated with irregular cycles, infertility, and insulin resistance, but one of the most overlooked aspects of PCOS is chronic inflammation. Inflammation plays a central role in PCOS, contributing to hormonal imbalances, metabolic dysfunction, and long-term health risks.
Understanding what drives inflammation in PCOS and how to manage it can make a significant difference in symptoms and overall well-being.
What Causes Chronic Inflammation in PCOS?
Inflammation is the body’s natural response to injury or infection, but in PCOS, the immune system remains in a low-grade inflammatory state even when no infection is present. Several factors contribute to this:
- Insulin Resistance: High insulin levels trigger the release of inflammatory markers like C-reactive protein (CRP) and cytokines, worsening inflammation and metabolic dysfunction.
- Excess Androgens: Elevated testosterone and other androgens promote inflammation and disrupt immune system regulation.
- Visceral Fat: PCOS often leads to fat storage around the abdomen, which releases inflammatory molecules that increase insulin resistance and hormone imbalances.
- Oxidative Stress: Increased levels of oxidative stress in PCOS lead to damage at the cellular level, fueling inflammation and worsening symptoms.
Gut Health Disruptions: Cause or Effect?
There is a growing discussion around the role of gut health in insulin resistance. Some suggest that an imbalanced gut microbiome may drive metabolic dysfunction, but the reality is more complex. The real problem is chronic inflammation caused by insulin resistance, which disrupts gut bacteria, not the other way around.
When insulin levels remain elevated, it creates a pro-inflammatory environment that alters gut permeability, damages beneficial bacteria, and allows harmful bacteria to thrive. This can further contribute to digestive issues and systemic inflammation. However, taking a probiotic alone will not fix the problem—lowering insulin levels and reducing inflammation is the key to restoring gut health.
Effects of Chronic Inflammation in PCOS
Persistent inflammation does not just contribute to PCOS symptoms—it also increases the risk of long-term health issues.
- Worsening Insulin Resistance: Inflammation makes insulin resistance more severe, leading to higher insulin levels and worsening metabolic health.
- Hormonal Imbalances: Chronic inflammation disrupts ovarian function, leading to irregular cycles, increased androgens, and difficulty with ovulation.
- Weight Gain and Fatigue: Inflammatory signals interfere with metabolism, making it harder to lose weight and contributing to persistent fatigue.
- Increased Cardiovascular Risk: PCOS already raises the risk of heart disease, and chronic inflammation further damages blood vessels, increasing the likelihood of hypertension and arterial plaque buildup.
- Fertility Challenges: Inflammation affects egg quality, implantation, and overall reproductive function, making it harder to conceive.
Managing Inflammation in PCOS
Reducing inflammation is key to improving symptoms and protecting long-term health. Here are the most effective ways to manage it:
1. Lower Insulin Levels: Since insulin resistance is a major driver of inflammation, keeping insulin levels stable is one of the most powerful ways to reduce inflammation. Avoiding insulin-spiking foods can help lower inflammatory markers and improve overall metabolic health.
2. Prioritize Anti-Inflammatory Foods: Focusing on whole, nutrient-dense foods that fight inflammation can make a big difference. Key choices include:
- Omega-3-rich foods like salmon, sardines, and flaxseeds
- Leafy greens and colorful vegetables high in antioxidants
- Nuts and seeds for healthy fats
- Olive oil and avocado for anti-inflammatory monounsaturated fats
3. Get Regular Movement: Exercise lowers inflammation and improves insulin sensitivity. Strength training and walking are particularly beneficial for reducing inflammatory markers while improving metabolic function.
4. Address Gut Health the Right Way: Instead of relying on probiotics as a quick fix, focus on the real issue: insulin resistance. Once insulin levels are under control, gut health can naturally improve.
5. Manage Stress and Prioritize Sleep: Chronic stress raises cortisol, which drives inflammation. Mindfulness, deep breathing, and getting at least seven hours of sleep per night can help regulate stress hormones and lower inflammation.
The Bottom Line
Chronic inflammation is a major driver of PCOS symptoms and long-term health risks. While gut health plays a role, the real issue stems from insulin resistance fueling inflammation—not the other way around. Probiotics alone will not fix the problem, but lowering insulin levels through A Low Insulin Lifestyle can reduce inflammation, improve gut health, and restore hormonal balance.
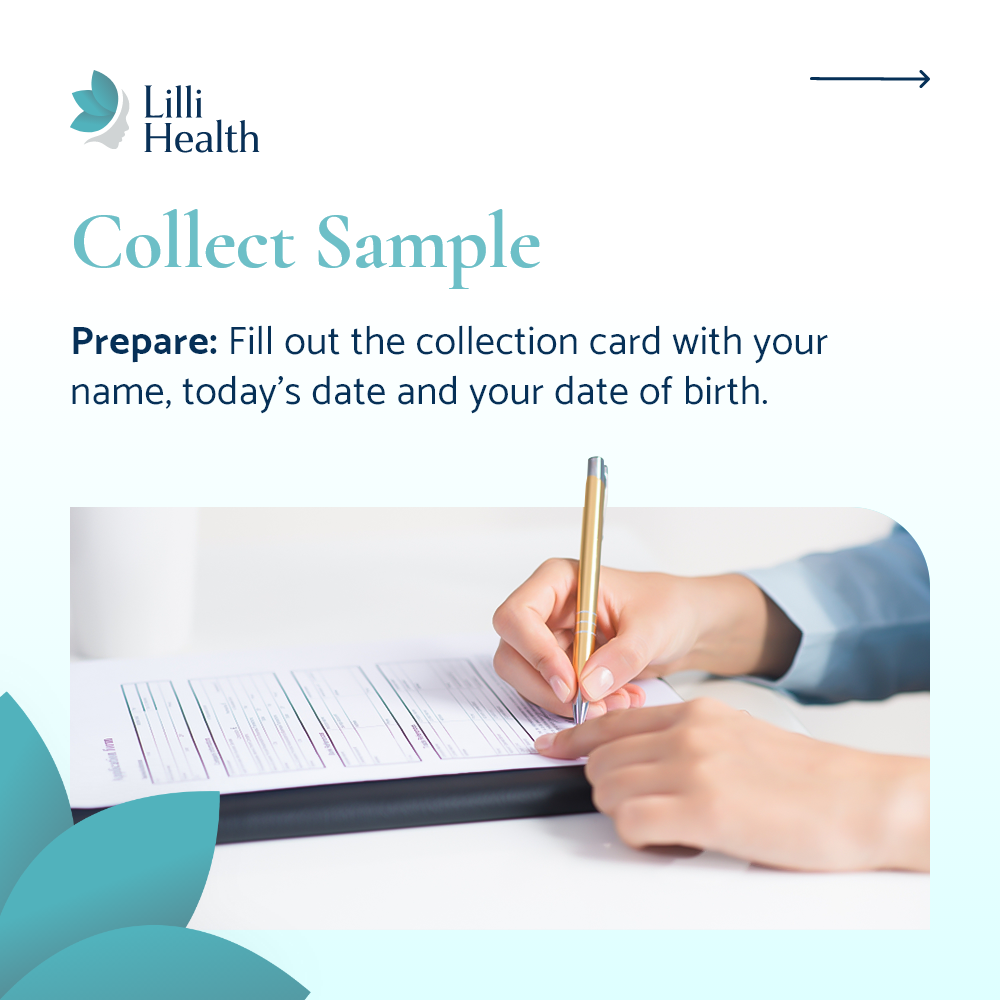
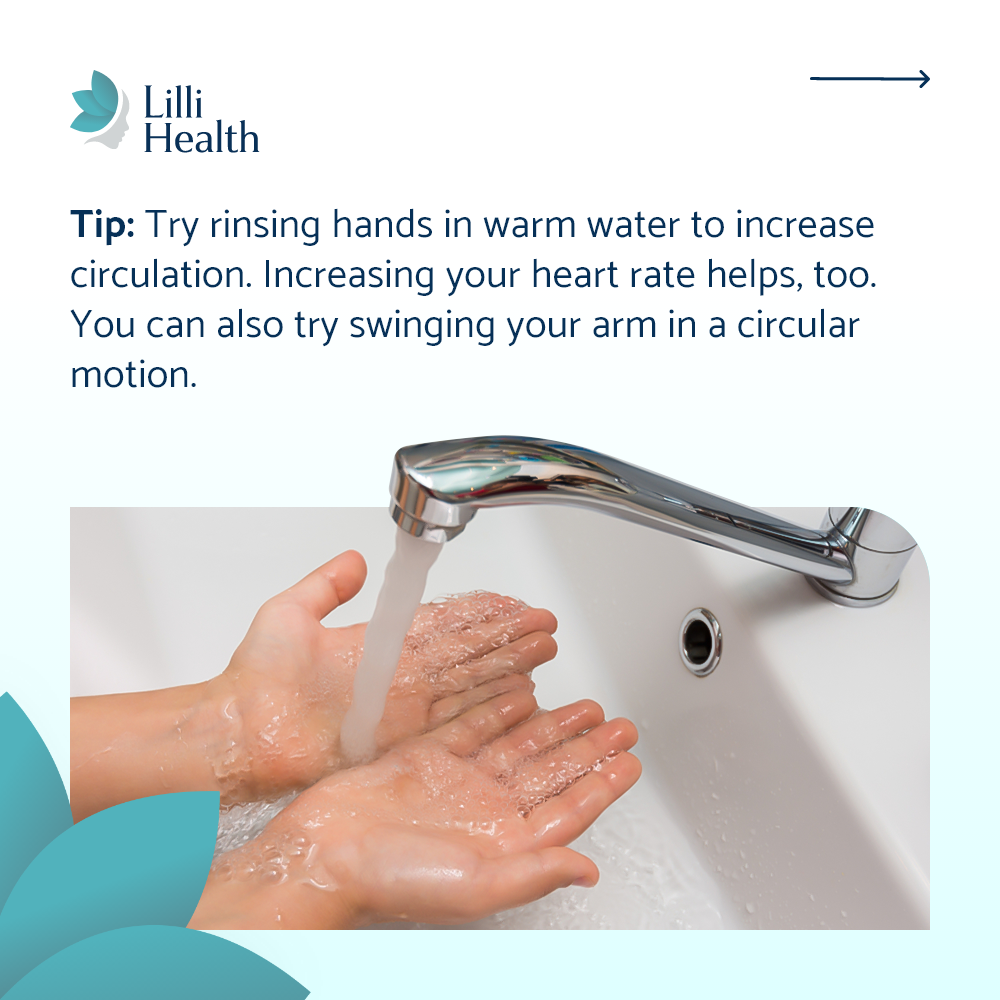
If you are looking for an easy way to track your metabolic health, Lilli Metabolic Testing Kits can help you measure your insulin levels and take control of your PCOS journey.