Insulin Resistance and Nutrient Deficiencies: Why Supplements Aren’t the Ultimate Solution
Insulin resistance is a pervasive issue that significantly impacts metabolic health, leading to various chronic conditions, including Polycystic Ovary Syndrome (PCOS), type 2 diabetes, and cardiovascular diseases. Alongside these conditions, nutrient deficiencies often arise, leading many to turn to supplements as a quick fix. However, while supplements can play a role in addressing nutrient gaps, they are not the ultimate solution. Understanding the relationship between insulin resistance and nutrient deficiencies reveals why lifestyle changes, specifically adopting a Low Insulin Lifestyle, are crucial.
The Link Between Insulin Resistance and Nutrient Deficiencies
Many essential nutrients, such as chromium, magnesium, and vitamin D, are depleted in the presence of insulin resistance and chronic inflammation.
Chromium and Magnesium: Insulin resistance and chronic inflammation can deplete these essential minerals. Magnesium is crucial for hundreds of biochemical reactions in the body, including energy production and muscle function. Chromium plays a role in carbohydrate and lipid metabolism. When insulin resistance is present, the body’s demand for these nutrients increases, leading to deficiencies.
Vitamin D: Unlike chromium and magnesium, vitamin D deficiency in insulin resistance is often due to excess fat storage. Fat cells absorb vitamin D from the blood, resulting in lower circulating levels. This is particularly problematic since vitamin D is vital for immune function, bone health, and inflammation regulation.
The Problem with Relying Solely on Supplements
While taking supplements can help replenish nutrient levels, they don’t address the underlying issue—insulin resistance. Simply put, supplements alone cannot rectify the metabolic imbalances caused by insulin resistance.
Symptom Masking: Supplements can mask symptoms temporarily without resolving the root cause. For example, taking magnesium might alleviate fatigue momentarily, but if insulin resistance persists, the fatigue is likely to return.
Temporary Fix: Nutrient supplements can offer a temporary fix but do not provide a long-term solution. For instance, vitamin D supplements can increase blood levels of the vitamin, but they don’t address why the deficiency occurred in the first place—excess fat storage due to insulin resistance.
Insulin Resistance: The Underlying Mediator
Many conditions associated with nutrient deficiencies are, in fact, conditions associated with insulin resistance. Insulin resistance often mediates the relationship between nutrient deficiencies and chronic symptoms or diseases.
Fatigue and Magnesium Deficiency: Fatigue is frequently attributed to magnesium deficiency. However, insulin resistance itself is a significant cause of fatigue. Insulin resistance leads to poor glucose utilization, resulting in reduced energy production and chronic fatigue. Thus, while magnesium supplements might provide temporary relief, addressing insulin resistance through lifestyle changes is necessary for sustained improvement.
Vitamin D and Chronic Conditions: Low vitamin D levels are linked to numerous chronic conditions such as osteoporosis and immune dysfunction. However, these conditions are also associated with insulin resistance. By improving insulin sensitivity, the body can better manage fat storage and improve vitamin D bioavailability, addressing the deficiency more effectively than supplements alone.
The Low Insulin Lifestyle: A Comprehensive Approach
Addressing insulin resistance at its core requires lifestyle changes that focus on reducing insulin spikes and improving metabolic health. The Low Insulin Lifestyle offers a holistic approach to managing insulin resistance and associated nutrient deficiencies.
- Dietary Changes: Prioritize whole, minimally processed foods that do not cause significant insulin spikes. This includes lean proteins, non-starchy vegetables, healthy fats, and whole fruits. Avoiding high-starch foods, milk and whey protein derivatives, and processed sugars is essential.
- Regular Physical Activity: Exercise enhances insulin sensitivity, helping the body manage glucose more effectively and reduce chronic inflammation.
- Stress Management and Sleep: Chronic stress and poor sleep can exacerbate insulin resistance. Incorporating stress-reduction techniques and ensuring adequate sleep are vital components of the Low Insulin Lifestyle.
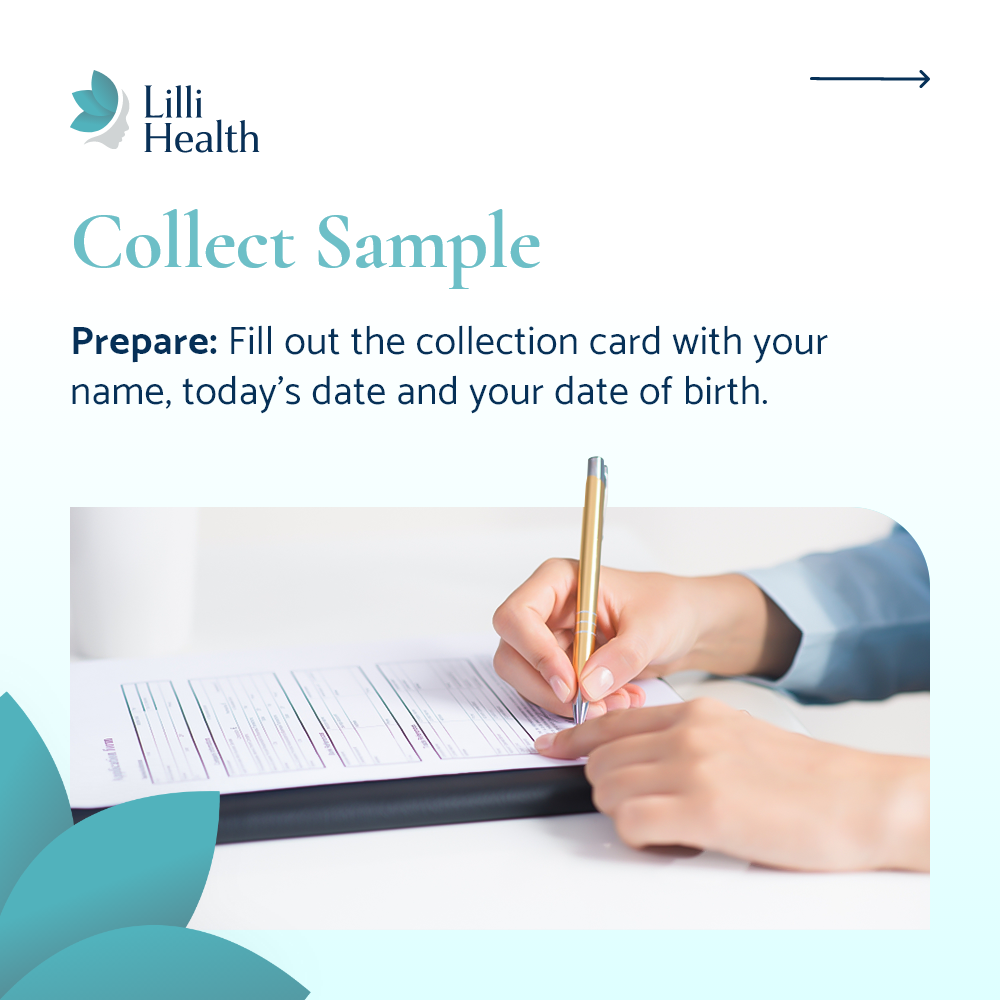
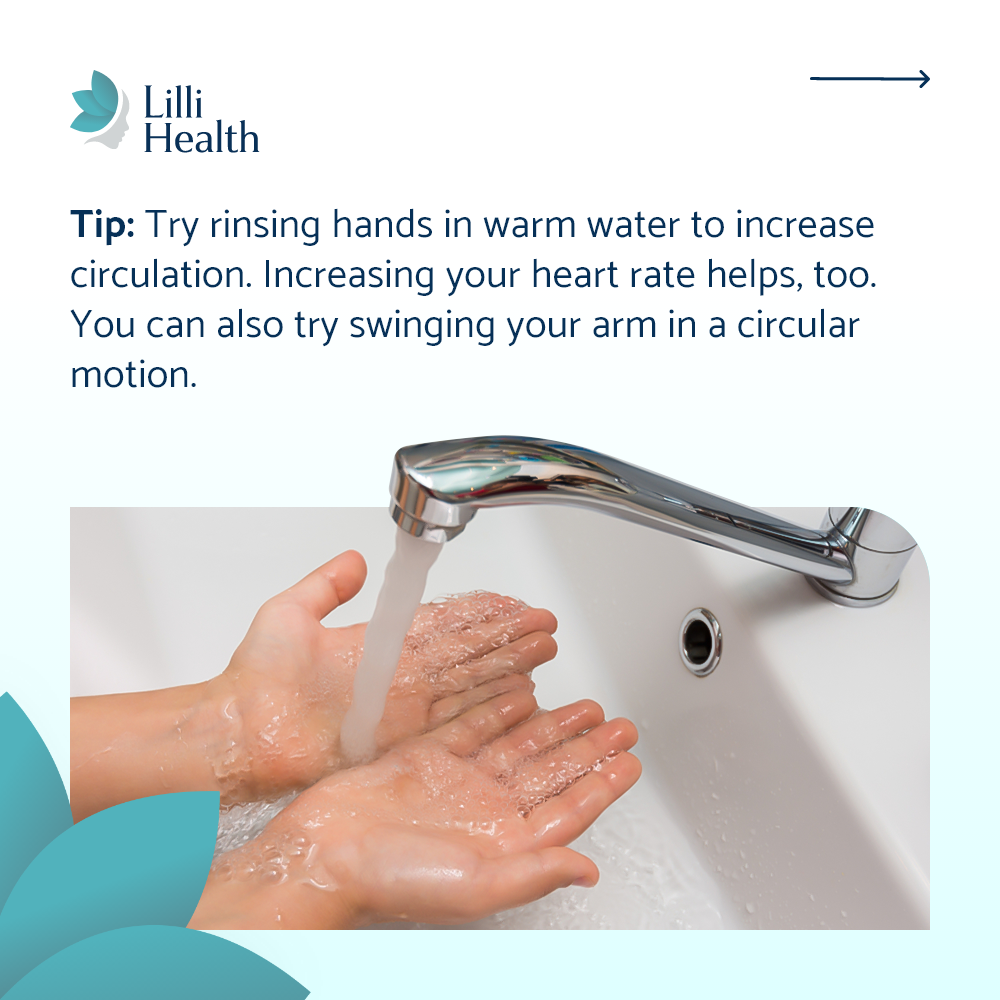
- Monitoring and Support: Using tools like the Lilli Health App can help track symptoms, monitor insulin levels, and provide educational resources to support a Low Insulin Lifestyle effectively.
Conclusion
While nutrient supplements can help manage deficiencies, they are not a standalone solution for insulin resistance and its associated conditions. Insulin resistance itself often mediates the relationship between nutrient deficiencies and chronic symptoms. Therefore, adopting a Low Insulin Lifestyle is crucial. This comprehensive approach addresses the root causes, offering sustainable improvements in metabolic health and overall well-being. For those struggling with insulin resistance and related nutrient deficiencies, focusing on lifestyle changes is the first and most critical step towards lasting health.