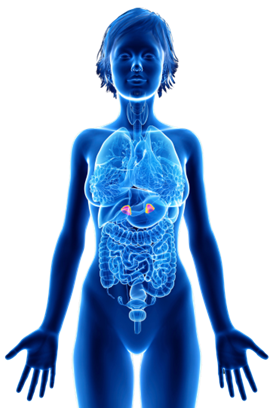
Insulin and fertility share a fascinating connection, which is essential to understand in order to navigate this aspect of reproductive health successfully. High levels of insulin and insulin resistance, a condition where our body’s cells become less responsive to insulin, have been linked to various fertility-related conditions, with polycystic ovary syndrome (PCOS) being one of them.
Women with PCOS often experience elevated insulin levels, which can disrupt the delicate balance of reproductive hormones like estrogen, progesterone, and testosterone. These imbalances can have repercussions on various aspects of fertility. For instance, high insulin levels have been linked to poor oocyte (egg) development and maturation. This can lead to lower egg quality, which in turn affects fertility and increases the risk of miscarriage. It’s like a domino effect!
But wait, insulin doesn’t stop there. It can also interfere with crucial processes like ovulation, implantation, and placental development. This means that high insulin levels can significantly impact a woman’s ability to get pregnant, maintain a healthy pregnancy, and reduce the risk of recurrent pregnancy loss.
In summary, high levels of insulin can:
- Interfere with the normal release of luteinizing hormone (LH), a key player in triggering ovulation.
- Impair the development and receptivity of the uterine lining, making it less welcoming for the fertilized egg to implant.
- Interfere with the normal development of blood vessels within the placenta, leading to potential pregnancy complications
“The link between insulin resistance and miscarriage is not new, but the culprit was thought to be blood glucose. Recent data suggests that it is actually insulin that’s causing damage to the placenta and that would change how we screen and treat women with recurrent miscarriage.”
Dr. Zev Williams, Director-Columbia University Fertility Center
The good news is that understanding the role of insulin in female infertility opens doors to potential interventions and treatments. By addressing insulin levels and improving insulin sensitivity, we can positively impact fertility outcomes. The bad news is that most women’s healthcare providers only test blood glucose and hemoglobin A1c levels, not insulin. By solely relying on blood glucose and A1c measurements, healthcare providers may miss the underlying insulin-related issues contributing to infertility and recurrent miscarriage. This can lead to missed opportunities for early intervention and tailored treatment plans that address insulin resistance and promote optimal reproductive function, such as a low insulin lifestyle.
Comprehensive insulin testing, which includes fasting insulin levels and HOMA-IR (homeostatic model assessment for insulin resistance), provides a more accurate assessment of a patient’s metabolic and reproductive health. It enables healthcare providers to identify insulin resistance or elevated insulin levels that may be impacting fertility.
In a published case series, infertile patients with PCOS were able to conceive on average 86 days after starting a low insulin lifestyle. That is unbelievable! By simply lowering their insulin levels, they were able to improve the health of their eggs, ovulate more regularly, create an improved environment for implantation, all of which improved their fertility.

It’s crucial to acknowledge that struggling to conceive can have various underlying factors, and there’s no one-size-fits-all solution. The beauty of adopting a low insulin lifestyle is that it’s a proactive approach you can integrate into your life alongside any other fertility treatments you may be pursuing. It complements and enhances the effectiveness of medical interventions, giving you the best possible chance of success on your journey to parenthood.
So, if you’re on the path to conception and searching for ways to enhance your fertility, consider the power of a low insulin lifestyle. Embrace the positive changes, stay determined, and keep that hopeful spirit alive. By nurturing your overall health and well-being, you’re setting the stage for a future filled with joy and the potential for new life.
We are thrilled to announce that soon we will be providing the Lilli at-home insulin testing kits directly on our website so that you can take this invaluable test in the comfort of your own home!
References
- Hoeger KM, Dokras A, Piltonen T. Update on PCOS: Consequences, Challenges, and Guiding Treatment. J Clin Endocrinol Metab. 2021;106(3):e1071-e1083. doi:10.1210/clinem/dgaa839
- Marshall JC, Dunaif A. Should all women with PCOS be treated for insulin resistance? Fertil Steril. 2012;97(1):18-22. doi:10.1016/j.fertnstert.2011.11.036
- Craig LB, Ke RW, Kutteh WH. Increased prevalence of insulin resistance in women with a history of recurrent pregnancy loss. Fertil Steril. 2002;78(3):487-490. doi:10.1016/S0015-0282(02)03247-8
- Ispasoiu CA, Chicea R, Stamatian FV, Ispasoiu F. High fasting insulin levels and insulin resistance may be linked to idiopathic recurrent pregnancy loss: A case-control study. Int J Endocrinol. 2013;2013. doi:10.1155/2013/576926
- Sharpe A, Morley LC, Tang T, Norman RJ, Balen AH. Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews. 2019;2019(12). doi:10.1002/14651858.CD013505
- Zhang D, Yang X, Li J, Yu J, Wu X. Effect of hyperinsulinaemia and insulin resistance on endocrine, metabolic and fertility outcomes in women with polycystic ovary syndrome undergoing ovulation induction. Clin Endocrinol (Oxf). 2019;91(3). doi:10.1111/cen.14050
- Balen AH, Morley LC, Misso M, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: An analysis of the evidence to support the development of global WHO guidance. Hum Reprod Update. 2016;22(6). doi:10.1093/humupd/dmw025
- Chen M, Li J, Zhang B, et al. Uterine Insulin Sensitivity Defects Induced Embryo Implantation Loss Associated with Mitochondrial Dysfunction-Triggered Oxidative Stress. Oxid Med Cell Longev. 2021;2021:1-18. doi:10.1155/2021/6655685
- Chang EM, Han JE, Seok HH, Lee DR, Yoon TK, Lee WS. Insulin resistance does not affect early embryo development but lowers implantation rate in in vitro maturation-in vitro fertilization-embryo transfer cycle. Clin Endocrinol (Oxf). 2013;79(1). doi:10.1111/cen.12099
- Araújo J, Cai J, Stevens J. Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009–2016. Metab Syndr Relat Disord. 2019;17(1):46-52. doi:10.1089/met.2018.0105
- Wang H, Zhang Y, Fang X, Kwak-Kim J, Wu L. Insulin Resistance Adversely Affect IVF Outcomes in Lean Women Without PCOS. Front Endocrinol (Lausanne). 2021;12. doi:10.3389/fendo.2021.734638
- Sun YF, Zhang J, Xu YM, et al. High BMI and Insulin Resistance Are Risk Factors for Spontaneous Abortion in Patients With Polycystic Ovary Syndrome Undergoing Assisted Reproductive Treatment: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2020;11. doi:10.3389/fendo.2020.592495
- Kelley AS, Smith YR, Padmanabhan V. A Narrative Review of Placental Contribution to Adverse Pregnancy Outcomes in Women with Polycystic Ovary Syndrome. Journal of Clinical Endocrinology and Metabolism. 2019;104(11). doi:10.1210/jc.2019-00383
- Kayemba-Kay’s S, Peters C, Geary MPP, Hill NR, Mathews DR, Hindmarsh PC. Maternal hyperinsulinism and glycaemic status in the first trimester of pregnancy are associated with the development of pregnancy-induced hypertension and gestational diabetes. Eur J Endocrinol. 2013;168(3):413-418. doi:10.1530/EJE-12-0609
- Riestenberg C, Jagasia A, Markovic D, Buyalos RP, Azziz R. Health Care-Related Economic Burden of Polycystic Ovary Syndrome in the United States: Pregnancy-Related and Long-Term Health Consequences. Journal of Clinical Endocrinology and Metabolism. 2022;107(2). doi:10.1210/clinem/dgab613
- Vega M, Mauro M, Williams Z. Direct toxicity of insulin on the human placenta and protection by metformin. Fertil Steril. 2019;111(3):489-496.e5. doi:10.1016/j.fertnstert.2018.11.032
- Spontaneous Pregnancies in Polycystic Ovary Syndrome (PCOS) Patients with a Low Starch/Low Dairy Diet: A Retrospective Case Series. J Community Med Public Health. 2022;6(2). doi:10.29011/2577-2228.100242