PCOS and Adrenal Health
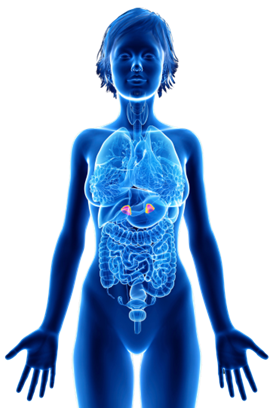
In PCOS, the body’s hormonal balance can be disrupted, leading to various symptoms like acne, excessive hair growth, and menstrual irregularities. One of the hormones involved in this condition is DHEA-S (dehydroepiandrosterone sulfate), which is produced by the adrenal glands located above the kidneys. DHEA-S is a precursor to testosterone and estrogen, and its levels are often measured in diagnosing PCOS.
Approximately 20-30% of women with PCOS have elevated levels of DHEA-S. While most excess androgens in PCOS come from the ovaries in response to high insulin levels, the adrenal glands can also contribute by producing excessive DHEA-S. Interestingly, elevated DHEA-S levels may also be associated with insulin resistance, further linking it to the development of PCOS.
Understanding the role of DHEA-S and its connection to insulin resistance provides valuable insights into the mechanisms behind PCOS. By addressing insulin levels and adopting a low insulin lifestyle, individuals with PCOS can work towards restoring hormonal balance and managing their symptoms effectively. It’s empowering to know that lifestyle changes can play a significant role in improving the overall well-being of those with PCOS.
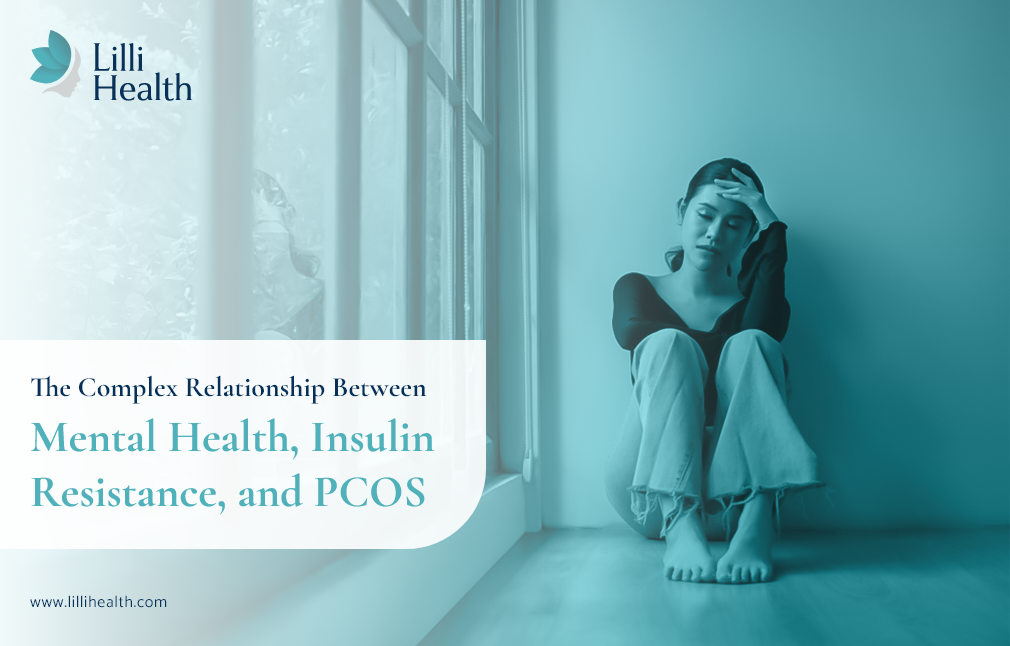
Stress
Stress and anxiety have significant impacts on our hormonal balance and overall well-being. When it comes to stress, the interplay between insulin resistance and cortisol is crucial to understand. Cortisol is produced by the adrenal glands in response to stress, and chronically high cortisol levels can lead to insulin resistance. Furthermore, high cortisol levels can contribute to overeating and weight gain, further worsening insulin resistance.
The increased insulin resistance not only contributes to rising insulin levels but also triggers the adrenal glands to produce excess androgens, such as testosterone. These androgens contribute to the signs and symptoms of PCOS, including acne, excessive hair growth, and menstrual irregularities. Therefore, managing stress is also an important component of a low insulin lifestyle.
Anxiety
In addition to the impact on insulin resistance, research has shown a potential association between insulin resistance and altered dopamine signaling in the brain, particularly in relation to mood disorders like anxiety. Dopamine, a neurotransmitter involved in mood regulation and motivation, may be affected by insulin resistance. Specifically, insulin resistance has been linked to decreased dopamine turnover, which refers to the rate at which dopamine is synthesized and metabolized in the brain. This decreased turnover may lead to decreased dopamine availability, which has been linked to depressive and anxiety symptoms.
Overall, chronic stress and anxiety can lead to overactivity of the adrenal glands, resulting in chronically elevated cortisol levels. This can contribute to a variety of health problems, including anxiety, depression, insomnia, and weight gain.
The good news is that through lifestyle changes and targeted interventions, we can tackle insulin resistance and its impact on adrenal androgen production. By adopting a low insulin lifestyle, including managing our stress, we can work towards improving insulin sensitivity and reducing the production of androgens from the adrenal glands. This comprehensive approach can help alleviate the symptoms of PCOS and promote better hormonal balance.
References
- Hoeger KM, Dokras A, Piltonen T. Update on PCOS: Consequences, Challenges, and Guiding Treatment. J Clin Endocrinol Metab. 2021;106(3):e1071-e1083. doi:10.1210/clinem/dgaa839
- Tsilchorozidou T, Honour JW, Conway GS. Altered Cortisol Metabolism in Polycystic Ovary Syndrome: Insulin Enhances 5α-Reduction But Not the Elevated Adrenal Steroid Production Rates. J Clin Endocrinol Metab. 2003;88(12):5907-5913. doi:10.1210/jc.2003-030240
- Kleinridders A, Cai W, Cappellucci L, et al. Insulin resistance in brain alters dopamine turnover and causes behavioral disorders. Proceedings of the National Academy of Sciences. 2015;112(11):3463-3468. doi:10.1073/pnas.1500877112
- Watson KT, Simard JF, Henderson VW, et al. Incident Major Depressive Disorder Predicted by Three Measures of Insulin Resistance: A Dutch Cohort Study. American Journal of Psychiatry. 2021;178(10):914-920. doi:10.1176/appi.ajp.2021.20101479
- Zou XH, Sun LH, Yang W, Li BJ, Cui RJ. Potential role of insulin on the pathogenesis of depression. Cell Prolif. 2020;53(5). doi:10.1111/cpr.12806
- Watson KT, Simard JF, Henderson VW, et al. Association of Insulin Resistance With Depression Severity and Remission Status. JAMA Psychiatry. 2021;78(4):439. doi:10.1001/jamapsychiatry.2020.3669
- Greenwood EA, Pasch LA, Cedars MI, Legro RS, Eisenberg E, Huddleston HG. Insulin resistance is associated with depression risk in polycystic ovary syndrome. Fertil Steril. 2018;110(1). doi:10.1016/j.fertnstert.2018.03.009
- Lyra e Silva N de M, Lam MP, Soares CN, Munoz DP, Milev R, de Felice FG. Insulin resistance as a shared pathogenic mechanism between depression and type 2 diabetes. Front Psychiatry. 2019;10(FEB). doi:10.3389/fpsyt.2019.00057