There seems to be so much focus on “regulating blood sugar” or “balancing blood sugar” these days. It can be confusing for people who have had their blood sugar tested, and the results came back normal. However, having blood sugars in the normal range doesn’t always tell the whole story. That’s because a standard blood sugar or hemoglobin A1c test can only tell you whether your blood sugar is too high, not if your insulin is too high.
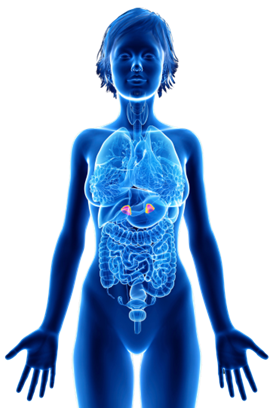
Insulin is the hormone that takes sugar from the blood and puts it into your cells so your body can use it for energy or store it as fat. When someone has high insulin levels, it means that the insulin they secrete doesn’t work correctly. If your insulin doesn’t work properly, the pancreas responds by making even more insulin. The pancreas will keep secreting as much insulin as it needs to eventually get excess blood sugars out of the blood and into the cells. It can’t just leave all that sugar in the blood; it’s toxic to organs!
All this excess insulin in the blood is a problem because high insulin levels lead not only to insulin resistance and fat storage but it also causes chronic low-grade inflammation.1–4 This inflammation affects every organ in your body.
Most people don’t understand that abnormal blood sugars are a symptom of a much bigger problem, high insulin levels. The worst part is that most people don’t even realize they have high insulin levels. It’s estimated that potentially up to 88% of adults have insulin levels that are too high and don’t even know it.5 This is because healthcare providers rarely measure insulin. Instead, healthcare providers only test blood sugar and hemoglobin A1c, which only tell you whether your blood sugar is high, not if your insulin levels are high. Someone could have high insulin levels for decades before finally having high blood sugar and getting diagnosed with type 2 diabetes.
 Check out this graph to see what I mean. This graph shows what you would probably see if you tested most adults’ blood sugar and insulin levels. You’d see a normal blood sugar level (blue) and a high insulin level (red) (the dotted line represents the threshold at which blood sugar rises high enough to warrant a diagnosis of Type 2 Diabetes).
Check out this graph to see what I mean. This graph shows what you would probably see if you tested most adults’ blood sugar and insulin levels. You’d see a normal blood sugar level (blue) and a high insulin level (red) (the dotted line represents the threshold at which blood sugar rises high enough to warrant a diagnosis of Type 2 Diabetes).
You could even think of the numbers in this graph by decades. In this scenario, you would be born with perfect metabolism, but by the time you are 20 or 30, insulin levels start to rise. At 50 years old, it really starts to get out of hand, and you may decide to get your blood sugar tested. Based on this graph, your blood sugar would be within the normal range, and you’d likely get a clean bill of health from your healthcare provider. This, as you can see, is not the complete picture. Your insulin level could be very high, and you not even know it. This is because most healthcare providers don’t test your insulin levels. In this example, your insulin started to rise in your 20s, and you would have spent your entire life with high insulin levels before you finally get diagnosed with type 2 diabetes. These high insulin levels are associated with everything from heart disease, Alzheimer’s disease, cognitive decline, infertility, and cancer.6,7
This is why having high insulin levels and insulin resistance is said to be a villain in an invisibility cloak. It lurks in the shadows, completely undetected. That is until it emerges in the form of disease.
Get your fasting insulin tested regularly and keep it low (between 3-8 mIU/mL).8 The best way to keep insulin levels low and maintain metabolic health throughout the lifespan is by following a low insulin lifestyle.9,10
References
- Zhang AMY, Wellberg EA, Kopp JL, Johnson JD. Hyperinsulinemia in obesity, inflammation, and cancer. Diabetes Metab J. 2021;45(3):285-311. doi:10.4093/DMJ.2020.0250
- Templeman NM, Skovsø S, Page MM, Lim GE, Johnson JD. A causal role for hyperinsulinemia in obesity. Journal of Endocrinology. 2017;232(3):R173-R183. doi:10.1530/JOE-16-0449
- Facchini FS, Hua NW, Reaven GM, Stoohs RA. Hyperinsulinemia: the missing link among oxidative stress and age-related diseases? Free Radic Biol Med. 2000;29(12):1302-1306. doi:10.1016/S0891-5849(00)00438-X
- Abdul-Ghani M, DeFronzo RA. Insulin Resistance and Hyperinsulinemia: The Egg and the Chicken. Journal of Clinical Endocrinology and Metabolism. 2021;106(4). doi:10.1210/clinem/dgaa364
- Araújo J, Cai J, Stevens J. Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009–2016. Metab Syndr Relat Disord. 2019;17(1):46-52. doi:10.1089/met.2018.0105
- Thomas DD, Corkey BE, Istfan NW, Apovian CM. Hyperinsulinemia: An early indicator of metabolic dysfunction. J Endocr Soc. 2019;3(9):1727-1747. doi:10.1210/js.2019-00065
- Janssen JAMJL. Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int J Mol Sci. 2021;22(15). doi:10.3390/ijms22157797
- Johnson JL, Duick DS, Chui MA, Aldasouqi SA. Identifying Prediabetes Using Fasting Insulin Levels. Endocrine Practice. 2010;16(1):47-52. doi:10.4158/EP09031.OR
- Phy Jennifer L, Pohlmeier AM, Cooper JA, et al. Low Starch/Low Dairy Diet Results in Successful Treatment of Obesity and Co- Morbidities Linked to Polycystic Ovary Syndrome (PCOS). J Obes Weight Loss Ther. 2015;05(02). doi:10.4172/2165-7904.1000259
- Pohlmeier AM, Phy JL, Watkins P, et al. Effect of a low-starch/low-dairy diet on fat oxidation in overweight and obese women with polycystic ovary syndrome. Applied Physiology, Nutrition and Metabolism. 2014;39(11):1237-1244. doi:10.1139/apnm-2014-0073