Polycystic Ovary Syndrome (PCOS) is a complex condition that affects many aspects of a woman’s health, from fertility to metabolic well-being. Unfortunately, misconceptions and misunderstandings surrounding PCOS abound, leading to ineffective advice and misguided beliefs.
In this blog, we’ll clear up a few of those myths to give you the truth about PCOS and women’s health. From managing weight to using birth control pills, let’s break down some common misconceptions about PCOS so you can feel more in control of your health.
Myth 1: “Eat Less and Exercise More”
The conventional approach to weight management, centered around caloric restriction and increased physical activity, is often insufficient for individuals dealing with PCOS. Contrary to prevailing wisdom, the oversight in this approach lies in neglecting a critical player in metabolic dynamics—insulin. For those with PCOS who frequently experience insulin resistance, addressing insulin levels is paramount to achieving effective and sustainable weight management.
Beyond its role in glucose regulation, insulin significantly influences weight and appetite control. Insulin resistance, a common feature of PCOS, results in the body’s cells being less responsive to insulin signals, leading to elevated insulin levels.
This, in turn, contributes to weight gain and heightened appetite, creating a challenging cycle that traditional weight management strategies may struggle to break. Therefore, a more holistic approach is needed, one that recognizes the intricate interplay between PCOS and insulin resistance, weight, and appetite.
Fact: PCOS weight loss starts with lowering insulin levels
Enter a Low Insulin Lifestyle—an evidence-based approach designed to lower insulin levels and facilitate weight loss in individuals with PCOS. This lifestyle modification involves making specific dietary choices to manage insulin response effectively. For instance, focusing on a diet rich in lean proteins, non-starchy vegetables, fruits, nuts and seeds, and healthy oils can help lower and maintain low insulin levels, contributing to PCOS weight management.
Myth 2: Hemoglobin A1c & Continuous Glucose Monitors Test for Insulin
While metrics such as Hemoglobin A1c and devices like Continuous Glucose Monitors (CGMs) are valuable tools in gauging overall metabolic well-being, they may not provide a complete picture when it comes to PCOS. One critical factor often overlooked in this context is insulin, a hormone that plays a pivotal role in PCOS and significantly influences metabolic dynamics.
Hemoglobin A1c, a marker reflecting average blood glucose levels over several months, and CGMs, which offer real-time glucose monitoring, are fundamental in understanding glucose regulation. However, PCOS is characterized by insulin resistance, wherein the body’s cells become less responsive to insulin signaling, leading to elevated insulin levels. Unfortunately, these conventional metrics may not directly account for the intricacies of insulin metabolism, leaving a crucial aspect of PCOS unexplored.
Fact: Testing specifically for insulin levels is critical
Insulin, beyond its role in glucose regulation, is intimately linked to the hormonal imbalances in PCOS. Elevated insulin levels can stimulate the ovaries to produce more androgens, exacerbating PCOS symptoms such as irregular menstrual cycles, acne, and hirsutism. Therefore, a more nuanced approach to metabolic health assessment in the context of PCOS demands a comprehensive evaluation of insulin levels.
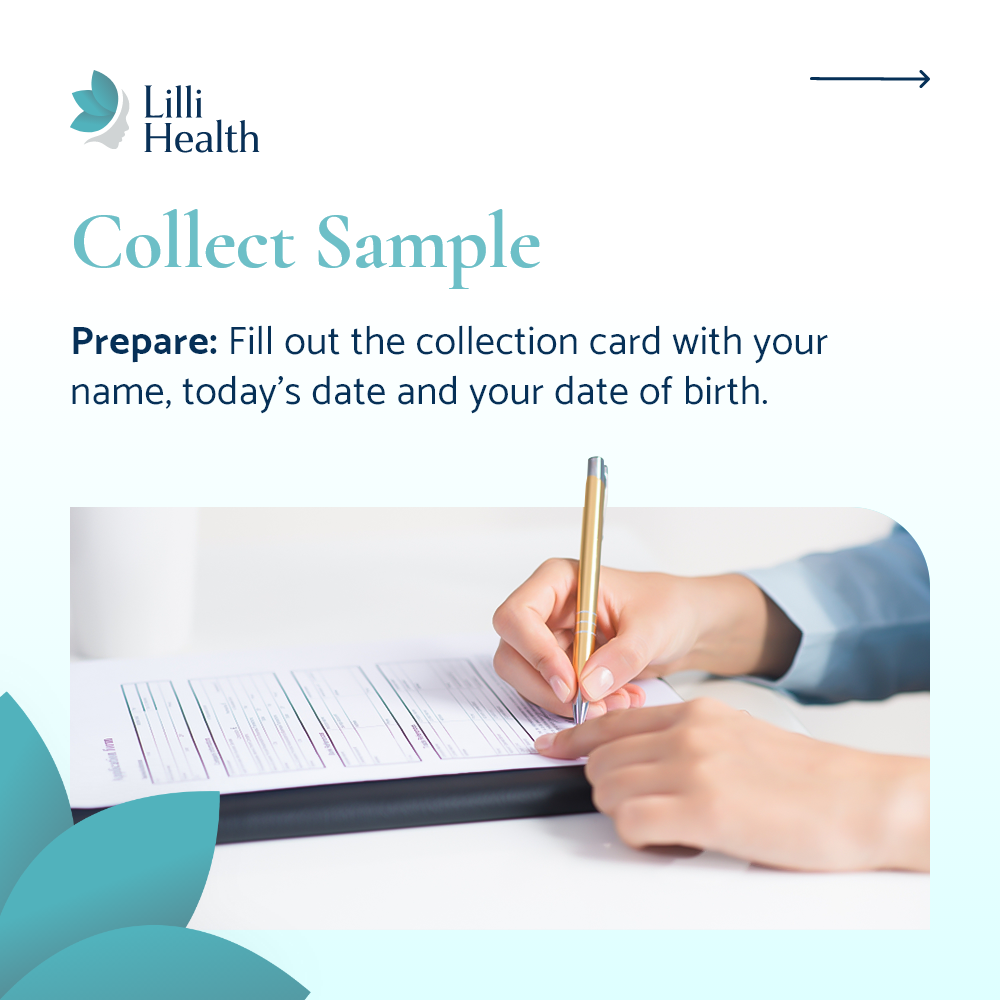
Evaluating insulin levels is essential for a holistic understanding of metabolic health in individuals with PCOS and insulin resistance. This may involve periodic insulin level assessments through blood tests. Monitoring insulin levels alongside traditional metrics can provide a more accurate representation of the metabolic challenges specific to PCOS. With the Lilli Insulin Testing Kits, you can measure your insulin levels from the comfort of your own home!
Myth 3: Birth Control Pills Cause or Cure PCOS
Birth control pills are frequently prescribed as part of the management strategy for individuals with PCOS, offering relief from a range of symptoms associated with this complex condition. While these pills don’t cause or cure PCOS, they play a crucial role in symptom management, providing substantial benefits that extend beyond regulating menstrual cycles.
Fact: Birth control pills can help with PCOS symptoms & mitigate risks
One of the primary symptoms addressed by birth control pills in the context of PCOS is irregular menstrual periods. PCOS often disrupts the normal ovulatory cycle, leading to irregular or absent periods. Birth control pills contain synthetic hormones, typically a combination of estrogen and progestin, which work by stabilizing hormonal fluctuations and inducing a predictable withdrawal bleed.
Beyond menstrual regulation, birth control pills contribute to alleviating other PCOS-related symptoms. These may include reducing the severity of acne and hirsutism (excessive hair growth), both of which can be exacerbated by the elevated androgen levels commonly seen in PCOS. By modulating hormone levels, birth control pills help restore a hormonal balance that addresses these pesky symptoms.
It’s important to note that the benefits of birth control pills extend beyond symptom relief. For individuals with PCOS, there is an increased risk of endometrial cancer due to prolonged exposure to unopposed estrogen, which can occur in the absence of regular ovulation.
Birth control pills mitigate this risk by providing a consistent, controlled hormonal environment that includes both estrogen and progestin. Progestin opposes the effects of estrogen on the endometrium, reducing the risk of hyperplasia (abnormal thickening of the uterine lining) and subsequent development of endometrial cancer.
Fact: Birth control pills can’t cure PCOS
However, while birth control pills offer significant advantages in managing PCOS symptoms and reducing associated health risks, it’s crucial to understand that they do not address the root cause of PCOS. These pills are a tool for symptom management, not a cure.
Therefore, individuals with PCOS, in consultation with their healthcare providers, should explore a comprehensive treatment plan that considers the broader aspects of PCOS, including lifestyle modifications such as a Low Insulin Lifestyle and, if necessary, additional medications targeting other symptoms or fertility concerns.
Myth 4: PCOS Causes Infertility
PCOS is commonly linked to ovulatory dysfunction, which can impact fertility. However, it’s essential to dispel the misconception that PCOS equates to infertility for every individual. Infertility is a multifaceted issue, and while approximately 30% of infertility cases arise from ovulatory dysfunction, within this category, PCOS accounts for around 80%. This underscores the importance of recognizing the diversity of factors contributing to infertility and the potential for successful conception in many cases of PCOS.
Fact: A Low Insulin Lifestyle can improve PCOS fertility
Lifestyle modification, such as a Low Insulin Lifestyle, is a powerful tool in addressing the ovulatory dysfunction associated with PCOS and improving fertility outcomes. A key focus of a Low Insulin Lifestyle is lowering insulin levels, a pivotal factor in PCOS-related infertility. Insulin resistance, prevalent in individuals with PCOS, can disrupt regular ovulatory cycles.
Implementing dietary changes that prioritize foods that do not spike insulin levels leads to lower insulin levels, reducing insulin resistance. Regular physical exercise complements these dietary adjustments, aiding in weight management and enhancing insulin sensitivity, further contributing to improved ovulatory function.
Fact: Insulin resistance can lead to higher miscarriage risk
In addition to the challenges associated with ovulatory dysfunction and fertility, individuals with PCOS may face an increased risk of miscarriage. The hormonal imbalances and metabolic irregularities characteristic of PCOS can contribute to a higher likelihood of early pregnancy loss. Insulin resistance not only affects ovulation but can also impact the early stages of pregnancy. Elevated insulin levels may create an environment less conducive to successful implantation and early fetal development.
Moreover, the associated hormonal imbalances, particularly elevated androgen levels, can influence the delicate balance necessary for a healthy pregnancy. Understanding this heightened risk emphasizes the importance of comprehensive care for individuals with PCOS who are trying to conceive, incorporating strategies not only to address ovulatory dysfunction but also to support a healthy early pregnancy.
Empowering women with PCOS with information about fertility management is crucial for navigating their reproductive journey. Understanding that fertility challenges associated with PCOS are often modifiable through lifestyle interventions fosters a sense of agency and hope. This empowerment extends beyond the individual to involve healthcare providers who can guide and support personalized approaches to fertility management.
Myth 5: You Caused PCOS
Let’s clear up a common misunderstanding: lifestyle choices or things you did or didn’t do caused your PCOS.
Fact: PCOS is caused by genetics and prenatal conditions
Contrary to erroneous beliefs, the prevailing understanding among experts is that genetic factors and prenatal conditions play a pivotal role in the development of PCOS. Research suggests that alterations in certain genes, possibly combined with environmental factors, contribute to the development of PCOS.
Specifically, the environment within the womb seems to be a critical factor, where exposure to high levels of testosterone and insulin during pregnancy can influence the development of PCOS later in life. This perspective shifts the narrative away from laying blame on lifestyle choices and behaviors, recognizing that PCOS is rooted in complex genetic and environmental interactions occurring before birth. This realization is empowering, as it helps free individuals of any undue self-blame and guilt.
Ultimately, the awareness that PCOS is not caused by personal choices promotes a more understanding and supportive community, paving the way for effective management strategies and improved quality of life for individuals affected by this common yet often misunderstood condition.
Key Takeaways: Debunking PCOS Myths
Dispelling common misconceptions about PCOS is crucial for fostering a more accurate understanding of this condition and improving the quality of care provided.
From the intricate interplay of insulin levels to the nuanced role of birth control pills, addressing PCOS requires a comprehensive and informed approach. By separating fact from fiction, we empower individuals with PCOS to navigate their health journey with knowledge, resilience, and the support they truly need.
Lilli Health’s Role in PCOS Management
A cornerstone of our mission at Lilli Health is to educate PCOS patients with evidence-based knowledge and proven treatment strategies so that they can take charge of their health and achieve better health outcomes that work for them.
While PCOS is a highly complex and nuanced condition, understanding the relationship between PCOS and insulin resistance is vital to seeking proper care and personalized treatment. Explore our other resources, including our Lilli Kits, newsletter, and upcoming Lilli app – all designed to help you effectively manage your condition, reclaim your well-being, and live a healthier, happier life.